Bruxism – involuntary clenching and grinding – can do serious damage to your teeth.
Treating bruxism before your teeth are worn to nubs may be the most underrated money-saving strategy in dental care. I wish many patients would take it more seriously! Alas, with human nature as it is, we often have to manage it after problems arise.
Some bruxers also develop temporomandibular disorder (TMD). TMD causes chronic headaches, jaw pain, crepitus, and restricted jaw movements.
Awake vs Sleep
There are technically two kinds of bruxism – awake bruxism and sleep bruxism. They are distinct disorders with distinct etiologies. But sleep bruxism causes significantly more damage to your teeth.
Click here to read my post about the differences between awake bruxism and sleep bruxism and the signs, symptoms, and causes of bruxism.
This post is focused on treatment.
Bruxism Treatment Considerations
Factors that determine whether and how we treat bruxism include:
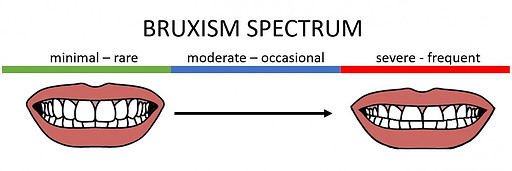
Severity – Bruxism occurs on a spectrum of severity from a mild intermittent disorder to an ongoing and severe one.
Pain – Some bruxers present with painful symptoms while others have no idea it’s happening. Painful symptoms compel patients to treat their condition. Those without pain may need more convincing.
Dental restorations – Bruxers with fillings, crowns, or veneers have a vested interest in protecting that work. Porcelain restorations cannot withstand bruxing forces as well as natural teeth. They can break, fracture, or debond under heavy loads.
Susceptibility to dental disease
- Periodontal disease – If you are prone to periodontal disease, the bruxism movements can intermittently open up the ligament space between the teeth and gums, enabling the periodontal pathogens access to this space. It is very common to see patients with bruxism develop periodontal disease.
- Cavities – If you are prone to cavities, keep in mind that you need enough healthy tooth structure available to place new restorations when they are needed. The attrition caused by bruxism can significantly reduce the tooth structure available to work with.
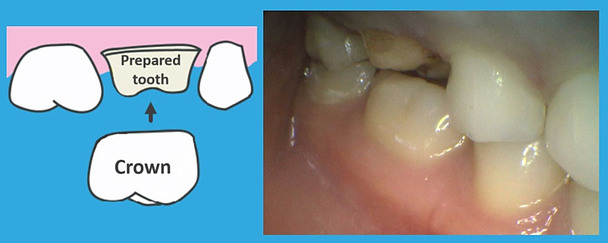
The above photo shows a crown preparation on a patient with sleep bruxism. Her teeth have significant attrition. The crown to be placed on this tooth will be prone to breaking or debonding for two reasons:
- This tooth had to be reduced more than ideal to accommodate room for the porcelain restorative material. The reduced surface area for bonding will make the crown vulnerable to debonding.
- If the patient continues to clench and grind at night without protection, the crown will be subject to repetitive heavy forces, and thus more likely to break or debond.
Of course, grinding itself can cause teeth to crack or fracture. Cracks and fractures are also reasons that teeth need crowns.
 Managing the restorative needs of a heavy bruxer is one of the biggest challenges in dentistry. Patients with extremely worn dentitions may need a dental specialist called a prosthodontist to elongate their teeth and rebuild their bite.
Managing the restorative needs of a heavy bruxer is one of the biggest challenges in dentistry. Patients with extremely worn dentitions may need a dental specialist called a prosthodontist to elongate their teeth and rebuild their bite.
Extensive restorative work like that can be very expensive – the cost is often comparable to the average annual salary in the United States! It is cost-prohibitive for many people.
Those who cannot afford this level of care are forced live with the consequences. Most people do not like the aesthetics of very short teeth. Worse yet, heavy bruxers are more likely to lose their teeth prematurely.
Who Requires Bruxism Treatment?
It goes without saying that anyone who is suffering from chronic jaw pain, headaches, or restricted movement will want to be treated. But patients with no painful symptoms may wonder if it’s anything to worry about.
Sleep Bruxism Without TMD Symptoms
You probably won’t require any treatment if you have mild asymptomatic sleep bruxism. The one exception is those with very delicate dental restorations. If you have porcelain veneers, for example, even an occasional episode of heavy bruxing could cause them to break or de-bond. If you have a significant investment in your smile, it is worth protecting it.
However, asymptomatic moderate to heavy sleep bruxers should always be treated. Patients often significantly underestimate the damage that sleep bruxism can do!
Awake Bruxism Without TMD Symptoms
Asymptomatic awake bruxers probably won’t do much damage to their teeth. They will not apply nearly the force that a sleep bruxer can.
However, if you notice that you clench and grind frequently, you have the potential to damage your muscles and joints and become symptomatic in the future.
For that reason, it is worth pursuing treatment to prevent damage and break this habit.
There is no surefire way to stop bruxism, but we have many tools to manage the condition.
Bruxism Treatments

Occlusal Guard
Most people are familiar with the first-line treatment for sleep bruxism – an occlusal guard. It is often called a night guard. An occlusal guard is a custom-fit appliance designed to fit over either your upper or lower teeth. It is typically made out of heat-cured acrylic or other hard plastic materials.
I recommend occlusal guards for patients who have sleep bruxism without pain or other TMD symptoms.
Fortunately, the majority of sleep bruxers do not have pain and can manage their condition with this simple appliance.
I do not recommend cheap off-the-shelf night guards as a long-term solution for sleep bruxism. They are either one-size-fits-all, or they use a boil-and-bite method. Either way, you won’t get a well-fitting or durable occlusal guard. It’s better to invest a little more into a higher quality guard that will last much longer and will do a better job protecting your teeth.
Do Night Guards Help Awake Bruxers Too?
Yes! If you are prone to clenching and grinding during the day, your jaw will be frequently over-closed beyond the ideal resting position. When your jaw is at rest, your teeth are comfortably apart. About 2 mm space separates the upper and lower teeth. An occlusal guard will help maintain that inter-dental space to keep your jaw in a more optimal resting position.
Since awake bruxers won’t apply as much force as sleep bruxers, their guards can be made from a softer and thinner material. Awake bruxers might even get away with an off-the-shelf style guard.
However, just like sleep bruxers – if awake bruxers already have painful TMD symptoms, an occlusal guard may not be the right solution.
The Purpose is to Protect Teeth
Some people reduce their bruxing motions with a standard occlusal guard, but most do not. A small percentage of bruxers with painful TMD symptoms will find relief with a standard occlusal guard, but most do not. Whenever I make a standard occlusal guard appliance, I am very clear to my patients. Its only function is to protect your teeth. If you are trying to prevent yourself from grinding or you are looking for relief from painful TMD symptoms, you will likely need another intervention.
TMD patients need specialized attention. They should not be treated by a general dentist unless he/she has specialized training in this area. I am a general dentist. I refer my symptomatic patients to a specialist.
A thorough discussion of occlusal guards and a review of various direct to consumer options is the subject of this post.
Pros and Cons of Occlusal Guard
Pros
- Reversible, non-invasive
- Protects teeth from wear and tear
- May help maintain a more optimal resting jaw position
- Cost – relatively inexpensive
Cons
- Requires compliance
- Some patients find it too uncomfortable to wear an appliance in their mouth
- Not a reliable treatment for symptomatic TMD patients
- Will not reliably prevent clenching and grinding motions
Shouting from the rooftops – the ideal time to get an occlusal guard is well before significant tooth wear!
As stated above, rebuilding your bite and your smile is extremely (often prohibitively) expensive.
Occlusal Splint
A common treatment for symptomatic TMD patients is a customized occlusal splint.
Bruxism is just one cause of TMD. TMD can also be caused by arthritis, injury, or other medical conditions. Bruxism-induced TMD is usually caused by overworked jaw muscles. Less commonly, pain is caused by damaged joints.
Like an occlusal guard, an occlusal splint will protect your teeth. But, unlike an occlusal guard, an occlusal splint is mainly designed to protect your muscles and joints.
On a standard occlusal guard, your opposing teeth touch evenly. As you clench and grind, your jaw moves around freely.
By contrast, an occlusal splint will not allow your jaw to move freely. Some are highly customized to your anatomy and physiology. They may have ramps to guide your jaw in specific directions to prevent damage to your muscles and joints.
Another type of specialized splint is called an NTI-tss. (or just NTI)
NTI-tss stands for – Nociceptive Trigeminal Inhibition – Tension Suppression System.
Are you still awake? Oh good. Don’t worry. You don’t need to understand what the name means. What’s important to know is that the NTI prevents you from clenching or grinding at all.
NTIs don’t cover all of your teeth in a given arch. They only cover a couple of your front teeth. You can’t clench or grind when your teeth have nothing to clench or grind against. Thus, your jaw muscles relax and no longer trigger inflammation and nerve hyperactivity. Your pain and headaches are relieved. It’s not just theory. Its effectiveness is substantiated by the evidence.
But, they do not come without downsides. Some people find that this small appliance falls out more easily. People who have worn an NTI for a long time can develop an open bite. In general, if the type of splint you wear does not cover all of your teeth, your uncovered teeth can shift.
Your provider will prescribe the type of splint that is appropriate for you and advise you when and how long to wear it. Sometimes it should be worn during the day, sometimes at night, and sometimes both.
Your provider will monitor you, adjust your appliance as needed, and manage complications. For splint therapy to work, you must be compliant and committed to follow-up.
These are some of the many reasons why custom occlusal splints must be prescribed by providers well-versed in this treatment. Treatment should be undertaken with a careful risk-benefit assessment.
A practical concern for patients is the cost of seeing a specialist. The good news is that oftentimes medical insurance will cover the treatments for TMD. A review of treatments that many medical insurance providers cover is detailed here. Occlusal splint therapy is often a covered procedure. Be sure to ask the provider you choose if he/she can bill medical insurance.
Pros and Cons of Occlusal Splint
Pros
- Reversible, non-invasive
- Protects teeth from wear and tear
- Often resolves painful TMD symptoms
- Sometimes covered by medical insurance
- Prevents bruxing motions or guides the jaw into less harmful motions
Cons
- Requires compliance and repeated follow-up with your provider
- Some patients find it too uncomfortable to wear an appliance in their mouth at night or during the day
- Some splints create conditions for teeth shifting
- If medical insurance does not cover it, it could be cost-prohibitive
- NTIs specifically are prone to falling out
Botox
Another promising treatment option is directing a small dose of botulism toxin (Botox) directly into your masseter muscles. Masseter muscles are the ones that move your lower jaw.
Botox will not stop you from grinding your teeth, but it will weaken the muscles and significantly reduce the force you exert – thus reducing wear and tear on your teeth, jaw pain, and headaches.
Some patients also notice a reduction in the size of their masseter muscles which softens their appearance.
The Botox injections must be repeated every three to six months for best results.
One potential concern about using Botox for TMD is that it may cause bone loss in the lower jaw. Clinical studies have demonstrated this effect.
Others find that bone loss is insignificant at low doses. Further research is needed.
Botox may be an option for TMD patients. Sometimes it is used as a stand-alone treatment. Other times, it is used in conjunction with appliance therapy.
It may also be appropriate for heavy sleep bruxers who cannot tolerate an occlusal guard.
Botox is not typically covered by dental or medical insurance to treat bruxism.
Pros and Cons of Botox
Pros
- If used as a stand-alone treatment, there’s no need to wear an appliance in your mouth
- Protects teeth and jaw by reducing bruxing force
- For some, it has a positive cosmetic effect
Cons
- Inconvenient – injections must be repeated every few months indefinitely
- Expensive – typically must be paid out-of-pocket
- Concerns about the long-term risk of bone loss
- Requires injections (a con for the needle-phobic)
Biofeedback
Biofeedback is the electronic monitoring of bodily functions to help people develop better control over them.
Bruxers can be alerted by a stimulus when they clench or grind to stop them in their tracks. Sometimes the monitors are embedded directly in an occlusal guard.
Biofeedback seems better suited to those with awake bruxism. Awake bruxers are semi-conscious of their clenching and grinding behavior. Repeated reminders to stop may eventually condition them out of it. It’s hard to believe that you can be conditioned out of sleep bruxism. It occurs while you’re not conscious of what you’re doing.
Nonetheless, there are biofeedback products that claim to work for sleep bruxism.
Proteeth guard makes a headband that alerts you with an audible tone when you grind your teeth at night. If you grind often, my concern is that you could have a very disrupted night’s sleep.
SOVN is a company that makes a device worn in your ear that vibrates when it detects bruxing motions. SOVN claims that the vibrations will stop you from grinding without waking you up. At the time of this post, this product has not been released to the market. We will have to wait and see how effective it proves to be.
If you’re trying to stop awake clenching and bruxing, you may not need to buy anything fancy. A conventional occlusal guard or an even an off-the-shelf bite guard can be used as a biofeedback-style deterrent. If you’re used to clenching your teeth together, the change in sensation may be enough to alert you to what you’re doing. It will also protect your teeth and help keep your jaw in a more optimized resting position.
Off-the-shelf guards may be useful for asymptomatic awake bruxers who are simply trying to stop their bruxing habit.
Research has not yet shown biofeedback to be reliably long-lasting for bruxism. However, it may work for some people. There is ongoing research in this area to improve the technique.
Pros and Cons of biofeedback
Pros
- Addresses the root cause
Cons
- Behavioral change has not yet been shown to be reliably sustainable over the long term
- Could be disruptive to sleep if used for sleep bruxism and is unlikely to reduce episodes of sleep bruxism
Treat Sleep Apnea if You Have It
Sleep apnea and sleep bruxism are positively correlated. One does not cause the other, but they are both triggered by the central nervous system. And it turns out that treating sleep apnea also decreases sleep bruxism.
Sleep apnea is a serious disorder. If you have any symptoms or risk factors for sleep apnea, I encourage you to get checked out. And if you treat your sleep apnea, you may solve your bruxism as well!
Common treatments for sleep apnea include a Continuous Positive Air Pressure (CPAP) device or a mandibular advancement appliance.
A sleep specialist will prescribe the CPAP. Most medical insurance plans will cover it.
Dentists with specialized training can make a mandibular advancement appliance. If you go this route, be sure to find a dentist experienced with this procedure. It can cause dental complications. Many medical insurance providers will cover the cost of the appliance. If you see a dentist, be sure he/she can bill medical insurance.
Pros and Cons of Treating Sleep Apnea
Pros
- You relieve two sleep disruptive disorders with one therapy
- CPAPs and mandibular advancement appliances are often covered by medical insurance
Cons
- The treatments prescribed for sleep apnea aren’t comfortable for everyone
Adjust Medications
Commonly prescribed medications that impact neurotransmitters are known to trigger or worsen bruxism. These include selective serotonin reuptake inhibitors (SSRIs) and medications used for ADHD like Adderall.
If an SSRI is causing your aggravating bruxism, Buspirone might help. Buspirone has been shown to reduce bruxism and relieve painful symptoms for patients on SSRIs. Of course, your doctor would have to determine if it is appropriate for you. And, you’d have to add another medication with potential side effects to your regimen.
Otherwise, you could try to work with your doctor to determine the risks and benefits of changing your medications to ones that do not have a bruxing side effect. In many cases, it’s not worth making the change.
Pros and Cons of Medication Adjustments
Pros
- Bruxism could be alleviated simply by changing or discontinuing medications – no appliance needed
Cons
- Adding new medications may come with undesirable side effects
- Stopping a medication may not be worth it – the therapeutic benefit of the medication may outweigh the benefit of relieving bruxism
Reducing Alcohol, Nicotine, and Caffeine
Alcohol, nicotine, and caffeine are enjoyed recreationally, but technically, they’re drugs. All three have been implicated in bruxism. Alcohol has the strongest effect of the three. Caffeine has the weakest. It takes about eight cups of coffee per day before the effect is noticed.
As we all know, alcohol, nicotine, and high levels of caffeine can cause other ill health effects.
You could abstain or reduce your consumption of these substances to enjoy better health overall and to help manage your bruxism.
Pros and Cons of Reducing Alcohol, Caffeine, and Nicotine
Pros
- You’ll enjoy other positive health effects aside from reducing bruxism
- Bruxism could be alleviated simply by reducing or abstaining from these substances – no appliance needed
Cons
- May not be realistic for everyone
- These substances are addictive and can be difficult to stop
Acupuncture/Massage
Acupuncture involves placing thin needles into certain points on the skin to relieve pain or to treat other physical or emotional conditions. Needle-phobics may be fearful of acupuncture, but most people find that it does not hurt.
Acupuncture is used an adjunctive therapy for bruxism-induced TMD. This study found that acupuncture relieved pain and tension in jaw muscles. It may also have other therapeutic benefits to relieve stress and anxiety. But, any effect will be temporary.
 Massage is also used as an adjunctive therapy for TMD. This study determined that patients who received both occlusal splint therapy and massage reported greater pain reduction.
Massage is also used as an adjunctive therapy for TMD. This study determined that patients who received both occlusal splint therapy and massage reported greater pain reduction.
Many people find acupuncture and massage to be enjoyable and relaxing. Medical insurance plans often cover these therapies for TMD patients. But, it will typically only cover a limited number of sessions per year. Repeating sessions beyond what insurance will cover (if any) may be cost-prohibitive.
Acupuncture and massage are helpful for many patients. They alleviate pain and stress and may help reduce awake bruxing. But they will not stop sleep bruxism and they are not reliable enough to recommend as stand-alone treatments.
Pros and Cons of Acupuncture/Massage
Pros
- May have additional therapeutic benefits aside from alleviating bruxism
- Many people find the experience to be enjoyable and relaxing
- Insurance often offers coverage for these therapies
Cons
- The effect will not be long-lasting – it requires repeated sessions to sustain
- Insurance coverage (if any) is likely to limit the number of sessions they will cover – it may be too expensive to continue
- Evidence for their effectiveness is not conclusive – not reliable enough to use as stand-alone treatments
- Needle-phobics may not tolerate acupuncture
Stress Reduction
If you are experiencing high levels of stress, it’s always a good idea to find ways to manage it. You could find a good therapist, exercise, meditate, spend more time with friends and family, or quit your job.
Reducing stress can help to alleviate awake bruxism symptoms. Stress is a known cause of awake bruxism.
But, reducing stress may not make a big difference for sleep bruxism. The role of stress in sleep bruxism is unclear. And, there is no evidence that engaging in practices designed to reduce stress will result in fewer episodes of sleep bruxism.
Pros and Cons of Stress Reduction
Pros
- You are more relaxed and at ease
- It may reduce symptoms of awake bruxism
Cons
- Unlikely to help with sleep bruxism
I hope this post helped you find the right approach for you. Even though there is no cure for bruxism, we have many ways to manage the condition. Sometimes just one therapy is needed. Other times you can try a combination of different approaches.
If you have bruxism, please be proactive. I’m especially nudging heavy bruxers who are not compelled by pain to seek treatment. Bruxism can do more serious damage than many people realize.
Feel free to share your experience with bruxism or ask a question by posting in the comment section below!



This is a horrible dental issue and my partner suffers from this. She now uses a guard to help alleviate the pain. So far this has worked. Not only is it painful for the person who has it but also for their partner! I have had many sleepless nights with my partner grinding her teeth but now, with the guard, I sleep a lot more!1
Is it common for people to just have sleep bruxism? My partner doesn’t grind when she is awake.
Thanks for all the info on this. If the guard stops working we now have plenty more treatments to try.
Tony
Yes, sleep bruxism and awake bruxism are distinct disorders with distinct etiologies. I’m so glad both you and your partner have found relief with a night guard! If you want more information about the cause, I review the current thinking in this post. https://informeddentalconsumer…