A vibrant, healthy smile and the ability to chew food comfortably are keys to a good quality of life. But they often go unappreciated until we’re on the verge of losing them.
Cavities are to blame for many dental problems. They are a major cause of tooth loss as well as untold pain and suffering. Not only that – they can be a major drain on your bank account!
If you want to limit the damage cavities can do to your life, you must understand them. Cavities may not be the most riveting topic, but please take the time to read this post. You will make more financially savvy dental care decisions and achieve a better outcome!
Understanding Cavities
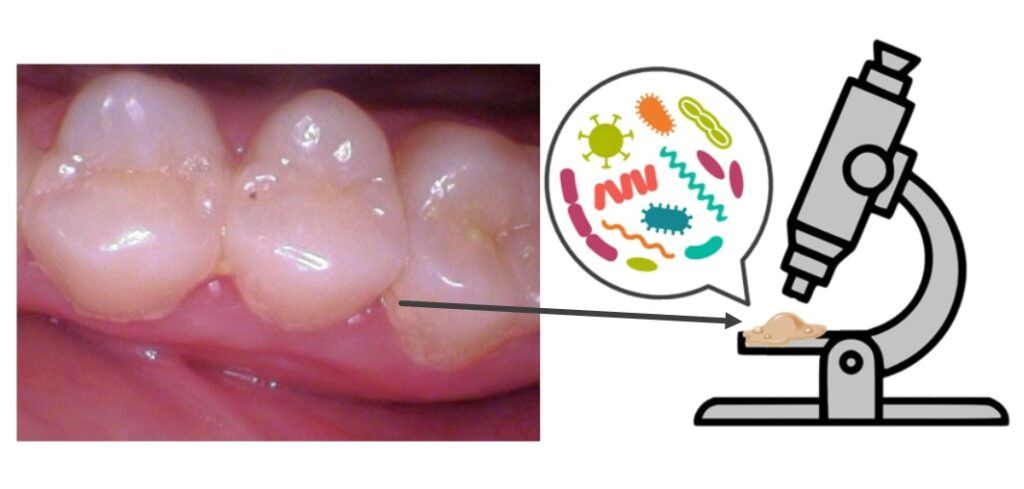
Most people understand that cavities are holes in teeth caused by dental plaque. But, they’re not just plain holes. They are mushy, sticky defects.
Dental plaque is nothing more than a gooey collection of bacteria and bacterial byproducts. The bacterial species that comprise your plaque vary from person to person.
Some cause cavities. Some cause gum disease. Others are friendlier.
As you may have already suspected, it’s not a fair system at all. There are many factors beyond your control that influence how susceptible you are to cavities.
These include the species of bacteria that comprise your plaque, the quantity, and quality of saliva you produce and your genetics. We are all somewhere on a spectrum of cavity susceptibility. 

As a side note, if you’re cavity-prone, don’t get too jealous! Those who are less prone to cavities aren’t off the hook. They might be at a greater risk for gum disease.
While cavities can occur anywhere, they can develop more easily in locations where dental plaque settles for a while.
Plaque often settles in pits and grooves on teeth chewing surfaces as well as in between teeth.
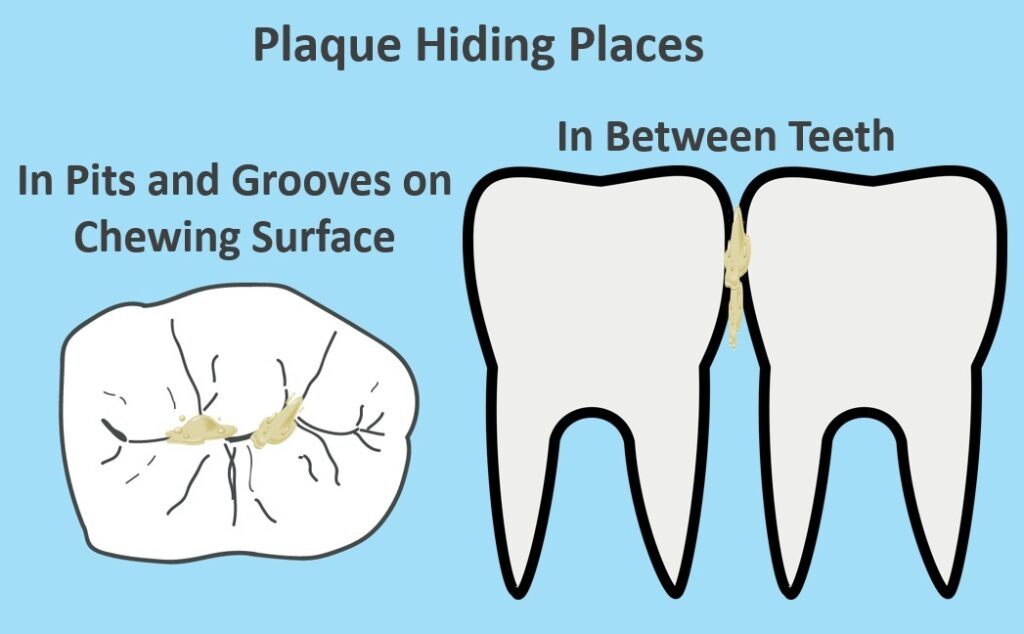

The rationale for placing dental sealants is to prevent cavities from initiating on the chewing surface. We seal the pits and grooves with resin and create a nice smooth surface.
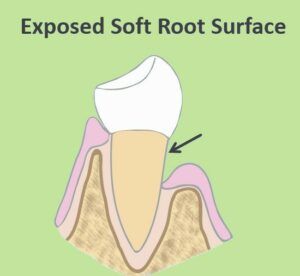
And finally, cavities also develop more easily on exposed roots. Because root surfaces are much softer than enamel they’re more vulnerable to developing cavities.
Cavity Causing Bacteria
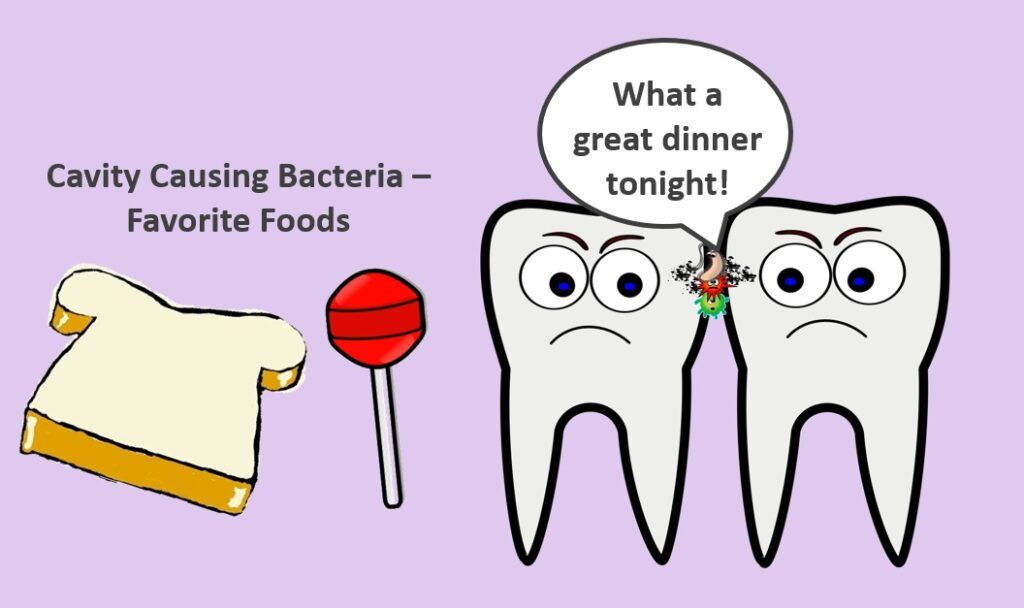
Cavity-causing bacteria love refined sugars.
While sticky sugary foods like lollipops are widely known to be bad for your teeth, even simple carbohydrates like white bread, pasta, chips, or crackers can feed these bacteria.
Their meals come from your leftovers. As they digest their food, they secrete a very acidic metabolic byproduct – in other words – bacteria poop.
Their acidic secretions destroy tooth structure and replace it with a sticky mush.
Counterintuitively, those who are the most cavity-prone often show little tendency to accumulate plaque. Even though plaque bacteria causes cavities, the acidic oral environment prevents large accumulations of plaque. I’ve seen many patients with super-clean looking teeth with many cavities.

The above photos show real-life examples of common cavity locations. If you can see them this easily, that means they’re quite big. We’d sure like to catch them a lot earlier.
Cavity Progression
Cavity progression can be broken down into four stages: 
- Stage 1 – small cavities
- Stage 2 – larger, deeper cavity
- Stage 3 – cavity reaches the pulp
- Stage 4 – cavity consumes too much of the tooth. It cannot be repaired

Stage 1
Stage 1 cavities are small – just at the threshold of detection. You won’t feel small cavities and you usually can’t even see them. We have to use tools to catch them.
To find early cavities that are starting on the chewing surface or other clinically accessible parts of a tooth, we use a dental explorer to check for sticky spots. Or we can use a special cavity-detecting laser to find those sneakier ones.

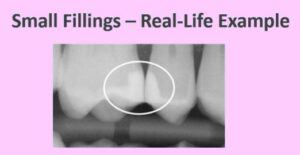
Dental x-rays help us find early cavities resulting from plaque settling between the teeth.

The x-ray above shows very small cavities as they show up on an x-ray. It’s those little dark spots. They are highlighted in yellow on the right. Without the x-ray, your dentist would have no idea that you have cavities. And, again, you wouldn’t have any symptoms like sensitivity. It is also the very best time to fix them.
Most of the time, stage 1 cavities are repaired with small fillings. Small fillings have a very low risk of post-operative discomfort or sensitivity.
The x-ray below shows a real-life example of small fillings. Easy breezy. Our patient went on the next day as if nothing happened.
But life with all of its distractions can keep us from the dentist sometimes. Dental care ends up on the back burner.
Unfortunately, cavities are unsympathetic. If unaddressed, they keep plowing through the tooth.
The rate of progression varies, but once the decay goes beyond the enamel layer and into the dentin, it will progress. 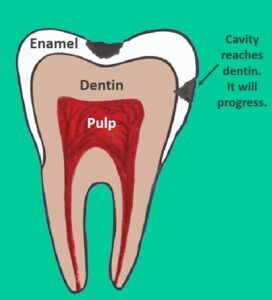
Once it does, you’ve reached stage 2.

Stage 2
At this stage, often, there is still no sensitivity. Stage 2 is the second best time to fix your cavity. A larger and deeper filling is required.
The greater percentage of your tooth that must be replaced by filling material, the weaker it gets. Weaker teeth are more vulnerable to cracks or fractures.
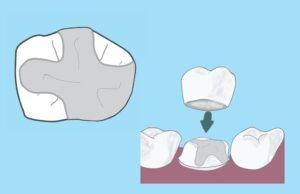
For larger fillings, it is often wise to upgrade to full-coverage crowns in order to prevent the potential for unpredictable infection or fracture.
 The deeper the filling, the closer it is to the tooth’s pulp. The pulp contains the sensory nerves of the tooth. It may become inflamed when a filling is placed close to it. There is a greater chance of prolonged sensitivity after a deeper filling is placed.
The deeper the filling, the closer it is to the tooth’s pulp. The pulp contains the sensory nerves of the tooth. It may become inflamed when a filling is placed close to it. There is a greater chance of prolonged sensitivity after a deeper filling is placed.
A cold drink can remind you it’s there. Of course, as stated earlier, the tooth probably did not hurt at all before the filling was placed.
Eventually, most of these super-sensitive teeth will get better. But, not always. Teeth with deeper fillings are at a greater risk for a pulp infection later. Read this post for more details.
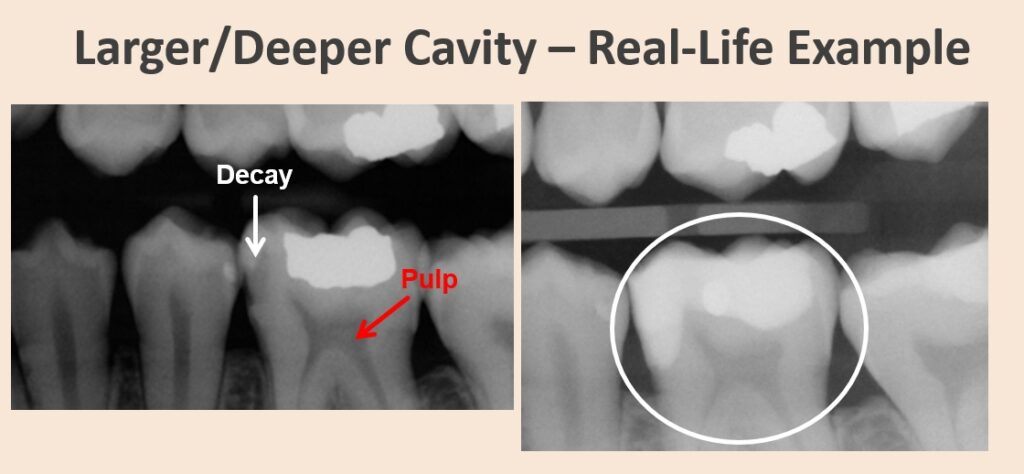
If life is still throwing those curve balls, and you can’t fix the cavity in stage 2, it will progress to stage 3.
 Stage 3
Stage 3
Once the decay – that mushy stuff – actually reaches the pulp, the pulp is officially exposed. And in order to save the tooth, we can’t even try a filling. It must get a root canal.
At this stage, believe it or not, most of the time, there is still no pain. Often there is some sensitivity when you eat something sweet or cold, but not always.
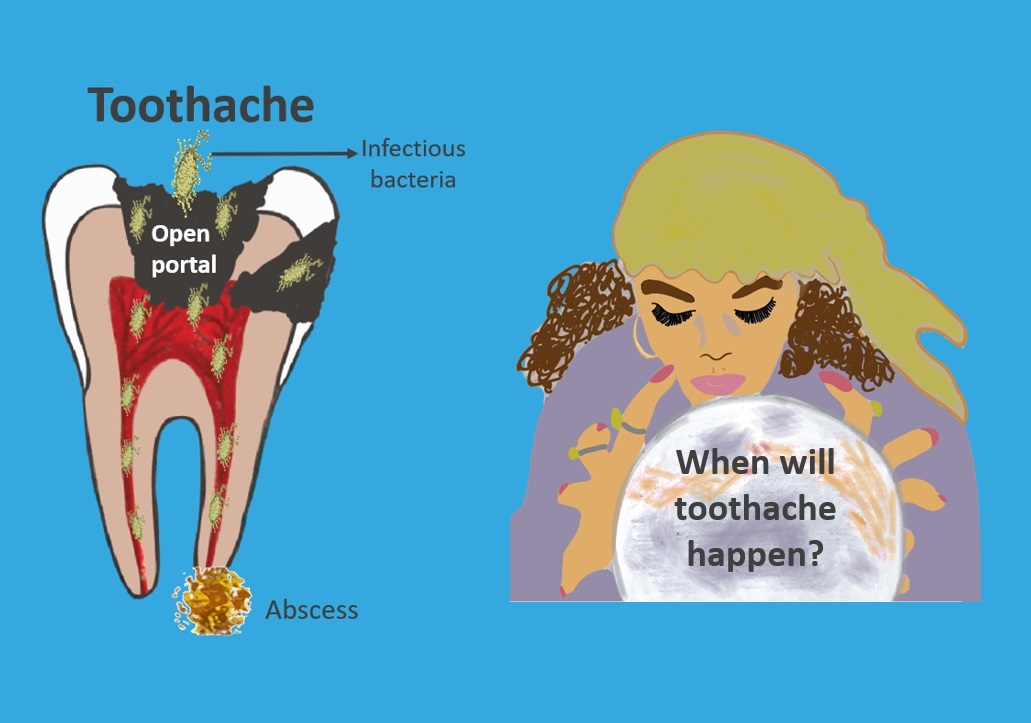
However, the tooth is at risk for a toothache. Excruciating toothaches typically develop as a result of an infection in the pulp.
The bacteria that cause this pulp infection are different than the ones that caused the cavity. However, the cavity allows a huge portal of entry right into the pulp.
When the pulp blows up with a big infection is anybody’s guess. But, please don’t wait for it!
A root canal involves removing the diseased pulp and nerve tissue, and then cleaning and shaping the empty canal space, and placing filling material in the canal space to seal it shut.
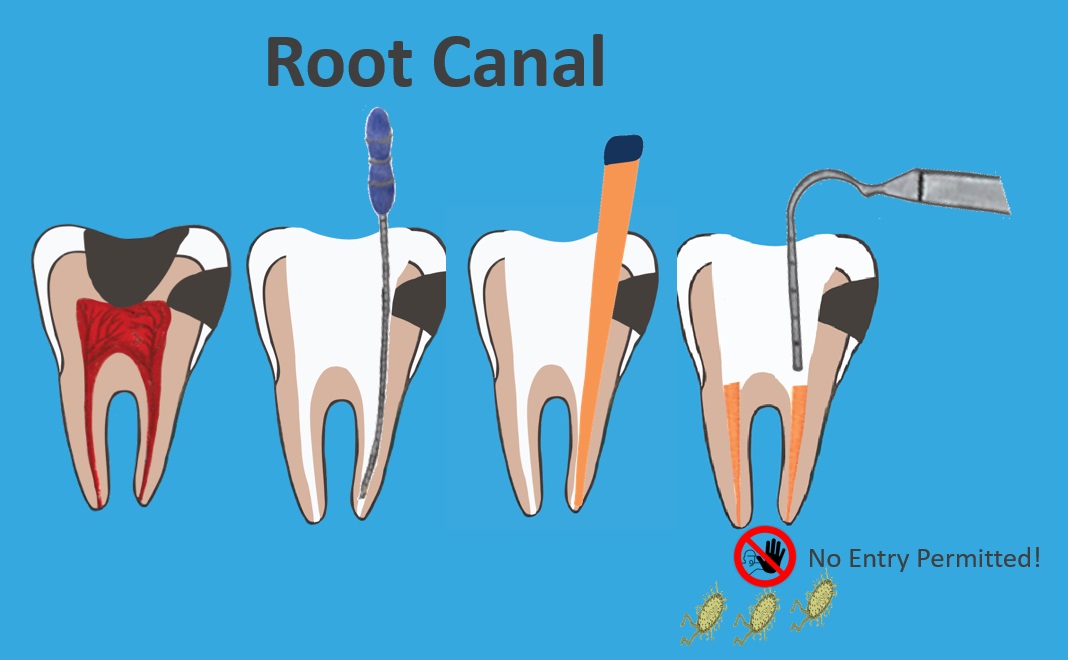
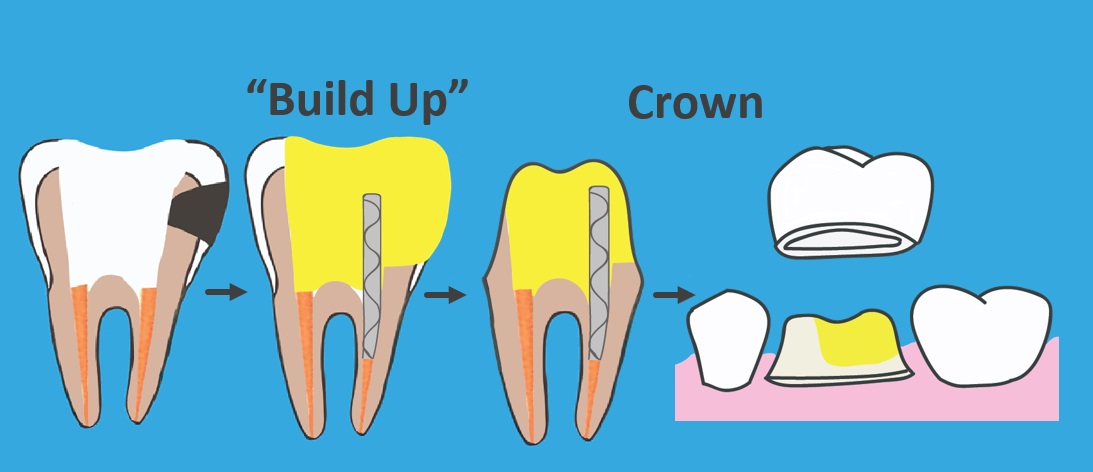
Once the root canal is complete, we’re not finished. The root canal only seals the root. The top part of the tooth still needs work.
- A build-up
- A crown
A build-up involves cleaning the cavity out of the top part of the tooth and replacing the diseased tooth structure with a filling. A post is sometimes used to better secure the filling.
After that is done, the tooth is healthy again. But after a root canal, teeth are more brittle and more prone to fracture. If it is a multi-cusped tooth, it should be covered and protected with a crown. Front teeth are not multi-cusped. Therefore, they do not always need a crown.
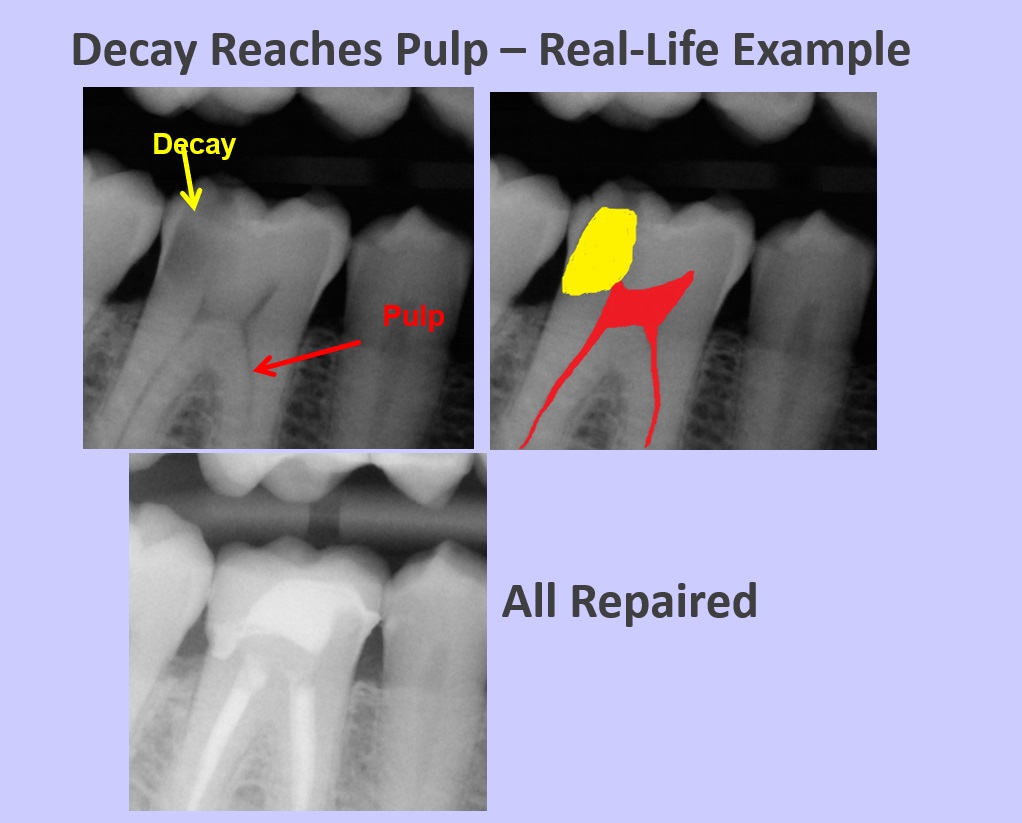
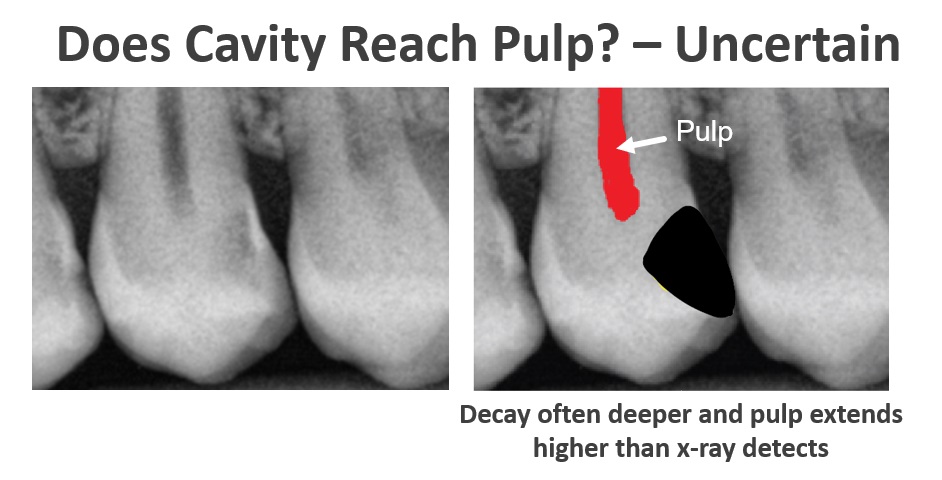
Real World Uncertainty
Sometimes an x-ray cannot tell us with certainty whether or not a tooth needs a root canal. X-rays are only so sensitive to pick up color variations. Decay is often deeper and the pulp is a little higher than can be visualized on an x-ray. Also, x-rays are two-dimensional representations of three-dimensional objects. So, sometimes, we won’t know whether a root canal is needed, or just a deep filling. We’ll find the answer when we’re in there.
 Stage 4
Stage 4
If we don’t get the work done in stage 3, the tooth will continue to decay and it will eventually progress to stage 4. Once the decay progresses too far, we can no longer fix the tooth. Our only option is to remove it.
Oftentimes, the nerves of teeth in stage 4 have already died, so they no longer register sensations like hot or cold, but they can still develop a painful infection at any time.

The image above shows the remains of teeth that never hurt badly enough to compel treatment. Again, don’t wait for pain!
The image below shows an example of the same tooth ten months apart. The tooth went from fixable to not fixable. The cavity destroyed too much of the tooth and it had to be removed. If you want to fix your tooth, don’t delay!

Luckily, in this day and age, we have many great ways to replace teeth.
But replacing a tooth is often more expensive than fixing one. To learn more about the ways we replace missing teeth, read this post.
After a dental exam, you may discover that you have quite a few cavities to address – cavities in all stages of development. Particularly if it’s been a while since your last dental visit.
That is when we need to be very strategic about your treatment plan. How to minimize your financial impact will be the subject of my next post. But, it’s very important to resolve your cavities one way or another. Once you do, be sure to see your dentist every six months for a check-up. That way you won’t develop a laundry list of needs again. You might have something pop up here or there, but it should be very manageable.
I hope it’s now crystal clear how staying ahead of tooth decay will save a tremendous amount of money, time, and pain over the course of your lifetime. Not to mention, the outcome will be much, much better!
Feel free to share your experience with cavities or ask me a question in the comment section below!


