Dental abscesses can be a very inconvenient and sometimes very painful interruption in our lives. They can also be dangerous if left to fester for too long. It’s important to cure your tooth abscess as soon as possible.
The treatment you need depends on the origin of your infection.
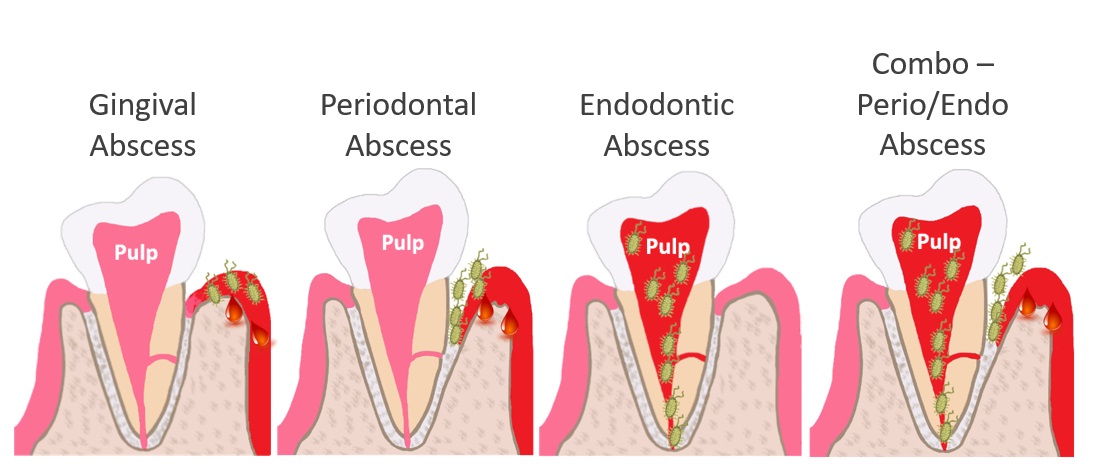
- Gingival Abscess – The infection origin is the gum tissue, and it is localized exclusively to the gums.
- Periodontal Abscess – The infection origin is in between the tooth and the gums and bone. It is deeper into the pocket than a gingival abscess
- Endodontic Abscess – The infection origin is inside the pulp. This is the most common type of tooth abscess.
- Combo Periodontic/Endodontic Abscess – Sometimes pathogenic bacteria from a periodontal pocket migrate inside the tooth and into the pulp. In this situation, the infection is in both the periodontal tissues and the pulp. Both sources of infection must be addressed.
Acute vs. Chronic Abscesses
Regardless of the infection origin, an abscess can be either acute or chronic.
- Acute – Acute abscesses are painful. Sometimes they cause swelling. The infectious exudate has built up and caused the area to throb or be extremely tender to touch. They are often managed with short-term measures to relieve pain and reduce swelling. We sometimes drain the abscess and/or prescribe antibiotics. Then we follow with definitive treatment. The treatment needed depends on the type of abscess you have.
- Chronic – Chronic abscesses can have very mild pain or no pain. That is because the pus has found a pathway out to drain so the pressure does not build. However, a chronic abscess has the potential to turn into a more severe infection without warning. When will it happen?
We have no idea! It could be days, months or many years! It is very important to treat all abscesses, whether acute or chronic.
Gingival Abscess
This type of infection is exclusively in the gum tissue. It does not penetrate down the periodontal pocket. It can be caused by a piece of food or a foreign object getting lodged in the gums, an injury to the gum tissue, or an accumulation of oral bacteria in the gum tissue. Sometimes the abscess ruptures by itself and requires no treatment. Otherwise, we can drain and clean the area. Warm salt water rinses are helpful during the healing phase.
If you have a gingival abscess, after it is resolved, be sure to follow up with regular care. You may have dental disease that predisposed you to develop a gingival abscess.
Periodontal Abscess
The periodontal abscess resides in between the tooth and the periodontal tissues. It extends beyond the gums and into the tooth-gum/bone attachment apparatus. The treatment for this type of abscess depends on the severity of the infection and the prognosis.
Etiology
 Cracked Root
Cracked Root
Occasionally a periodontal infection can be caused by a cracked root. A crack will destroy the attachment apparatus of the tooth so that it can’t attach to the gums and bone in the area of the crack. Infectious bacteria accumulate in the pocket defect created. A tooth with a periodontal abscess caused by a cracked root cannot be saved. It must be extracted.
Periodontal Disease
But far more commonly, an acute periodontal abscess is caused by an exacerbation of pre-existing periodontal disease.
Treatment
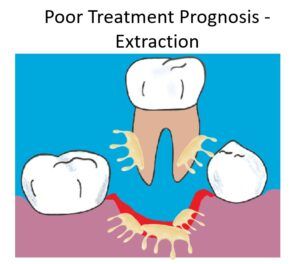 If the prognosis is poor, the only way to resolve your periodontal abscess is to extract your tooth. Even though the tooth itself is not infected, the tooth is required to sustain the periodontal infection. That is because the bacteria live in between the tooth and periodontal tissues. Once the tooth is gone, the bacteria have no place to live. The infection is cleared.
If the prognosis is poor, the only way to resolve your periodontal abscess is to extract your tooth. Even though the tooth itself is not infected, the tooth is required to sustain the periodontal infection. That is because the bacteria live in between the tooth and periodontal tissues. Once the tooth is gone, the bacteria have no place to live. The infection is cleared.
If your tooth can be saved, it will require periodontal therapy.
Periodontal Therapy for Periodontal Abscess
There are many periodontal treatment modalities available. The treatment needed may be as simple as a non-surgical deep scaling of the infected tooth. More severe cases may require surgery. Adjunctive therapies like lasers or antibiotics delivered directly into the pocket can also be used.
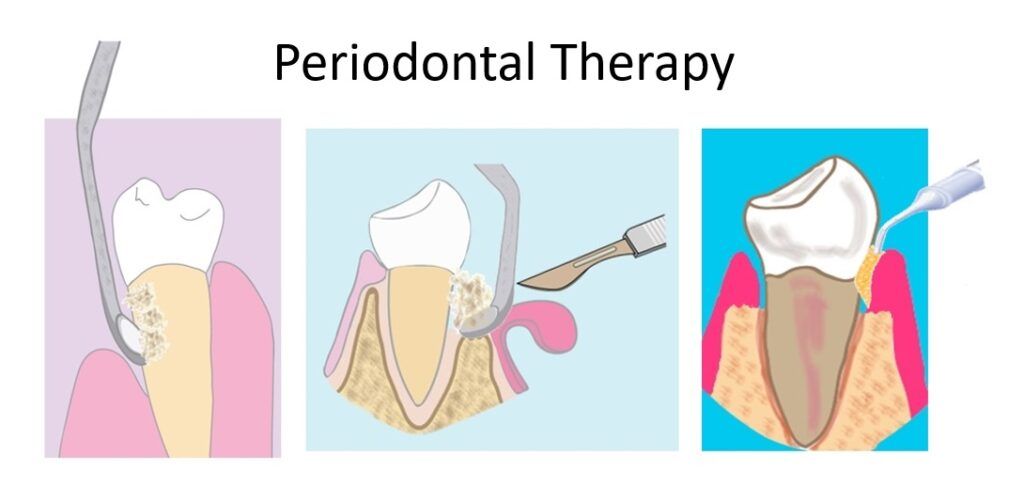 If you have a periodontal abscess it’s usually not the only tooth affected by periodontal disease. So, you will likely need a comprehensive solution to manage it. Read this post to learn more about periodontal disease and available treatment.
If you have a periodontal abscess it’s usually not the only tooth affected by periodontal disease. So, you will likely need a comprehensive solution to manage it. Read this post to learn more about periodontal disease and available treatment.
Endodontic Abscess
The endodontic abscess is the classic and most common dental abscess. When generically referring to a tooth abscess, we usually mean an endodontic abscess. They are also called peri-apical abscesses. That is because the infection accumulates around the apex of the root. The source of infection is the pulp.
A pulp infection has to reach a level of severity before any signs or symptoms of an endodontic abscess develop.
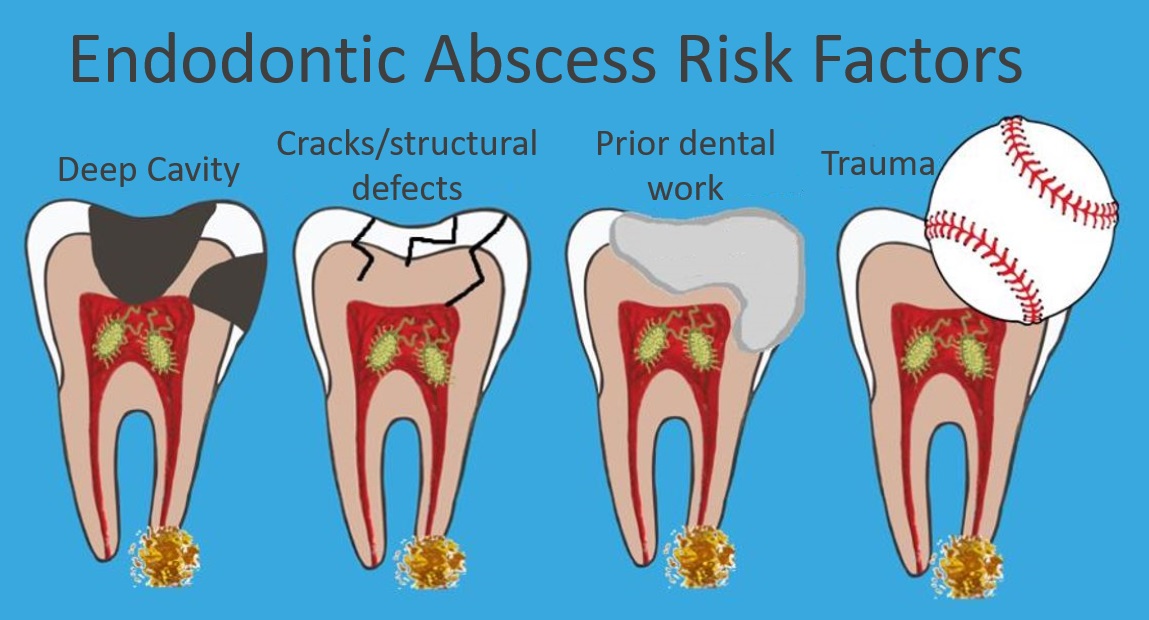
Risk factors for developing an endodontic abscess include
- A deep cavity – A deep cavity is the most common reason for an endodontic abscess. The bacteria that cause a cavity are not the same ones that cause an abscess. But the cavity allows a huge portal of entry for these infectious bacteria into the pulp.
- Cracks or other structural defects – Similar to a deep cavity, the cracks or defects allow bacteria an easier pathway to infect the pulp.
- Prior dental work – The trauma of dental work like deep fillings or crowns can cause a pre-existing, low-grade, asymptomatic pulp infection to flare up into a diagnosable endodontic abscess. Or, it can cause the pulp to become inflamed and eventually die. Dead pulps are more vulnerable to infection. (to learn more click here)
- Prior trauma to the tooth – Just like dental work, physical trauma to a tooth can also cause the pulp to become inflamed and die. Sometimes it takes months or years after the traumatic incident before a diagnosable infection develops.
Endodontic Abscess Diagnosis – Signs vs. Symptoms
We use signs or a combination of signs and symptoms to diagnose an endodontic abscess.
Signs – Signs are objective. They are phenomena that an outsider can detect. Signs offer the best diagnostic evidence.
Symptoms – Symptoms are subjective. Only you can experience your symptoms.
X-Ray Sign
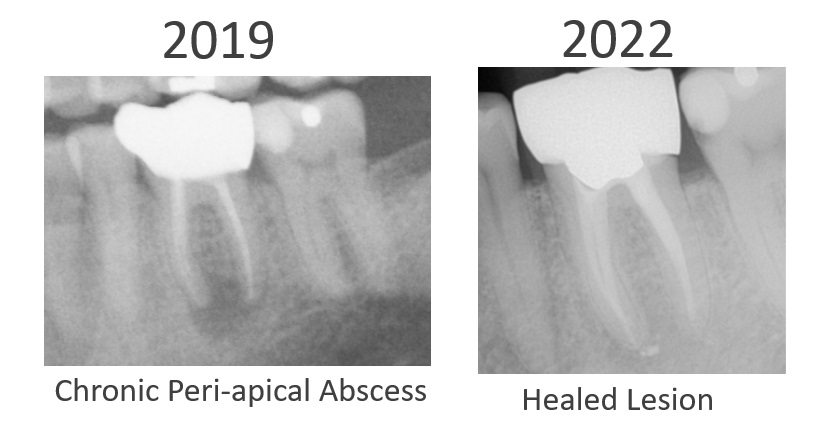
 A classic sign of an endodontic abscess visible on an x-ray is a dark spot at the tip of the root. The presence of a dark spot is definitive evidence of an abscess. However, the absence of a dark spot does not rule out an abscess.
A classic sign of an endodontic abscess visible on an x-ray is a dark spot at the tip of the root. The presence of a dark spot is definitive evidence of an abscess. However, the absence of a dark spot does not rule out an abscess.
Sometimes a tooth that presents that way has a chronic abscess that causes no pain. The abscess is a complete surprise. Other times, the patient is in agony with an acute abscess and the diagnosis is no surprise at all! But, from the outsider’s point of view, it can look the same whether acute or chronic.
Clinical Signs
Another definitive sign of an abscess is the presence of a draining fistula. The infection has found a pathway out, but the pus continues to build up and drain. These are often chronic and painless.
It’s worth reminding – chronic abscesses have the potential to flare up into a much more severe infection at any time.
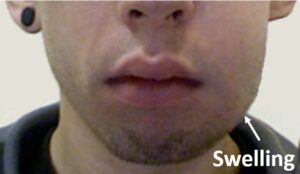
Another easily identifiable sign of an abscess is swelling. Sometimes the swelling is inside the oral cavity in the gum area near the affected tooth. Other times you have large extra-oral swelling visible on your face – the kind a stranger would notice.
Symptoms
If we don’t see an obvious sign of an abscess, we can sometimes diagnose it on the basis of your symptoms. Acute abscesses often present with spontaneous throbbing of the affected area. The pain often radiates well beyond the affected tooth. You feel it in your head or jaw. It’s usually severe enough to prevent you from sleeping. Often the pain comes and goes. It can subside for a day or two before returning with a vengeance. If you present with these symptoms and your painful tooth has obvious risk factors for an endodontic abscess, we can confidently conclude you have one.
Sometimes symptoms or signs are not definitive enough to know for sure whether or not you have an abscess. In that case, your dentist may have you wait it out to see if your symptoms subside or progress. Or, your dentist may refer you to a specialist called an endodontist for a more thorough evaluation. Endodontists typically have cone beam imaging capabilities which can sometimes pick up abscesses when x-rays can’t.
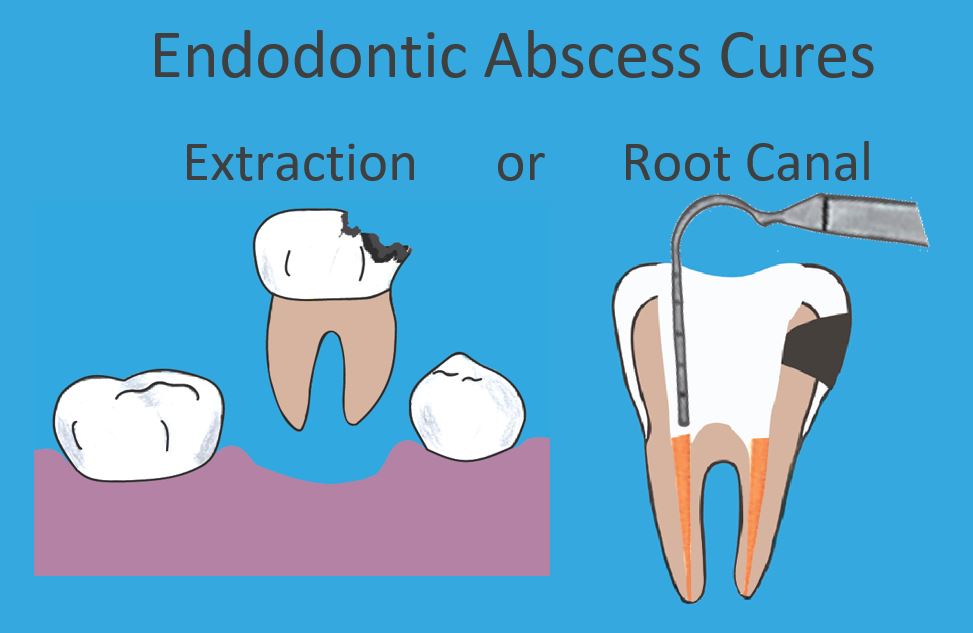
Treatment for Endodontic Abscess
The treatment to cure an endodontic abscess is either a root canal or extraction. That’s it! There are no other options. If the prognosis of treatment is poor, then the tooth must be extracted. Otherwise, you have the choice between a root canal or extraction.
 Antibiotics – Not the Answer
Antibiotics – Not the Answer
If you have an endodontic abscess, antibiotics will not solve your problem. Antibiotics are never, ever, ever a cure for an infected pulp. It’s important to definitively take care of your infection as soon as possible.
As stated earlier, antibiotics are sometimes needed prior to definitive treatment to manage swelling and pain.
They may temporarily reduce the part of the infection that has extended beyond the tip of the root. The throbbing and pressure may subside for a while. But, antibiotics cannot penetrate the source of the infection – the pulp. If the infection is not ultimately resolved with either an extraction or root canal, it will return. The next time it is usually worse.
Some people repeatedly request antibiotics for the same tooth. That is dangerous. The longer the infection is present, the more likely it evolves into more virulent strains of bacteria and spreads to other parts of the body. People have died from dental abscesses. It’s not common, but it’s not something to mess around with!
Treat your infection definitively as soon as possible.
Root Canals Explained
Since the source of the infection is the pulp of the tooth, to clear the infection we need to remove the pulp. But we can’t leave a large empty space in the middle of your tooth. Otherwise, bacteria would colonize that empty space. So, we must disinfect the pulp space and seal it off with a filling. To do so, we use a rubbery filling material called gutta-percha.
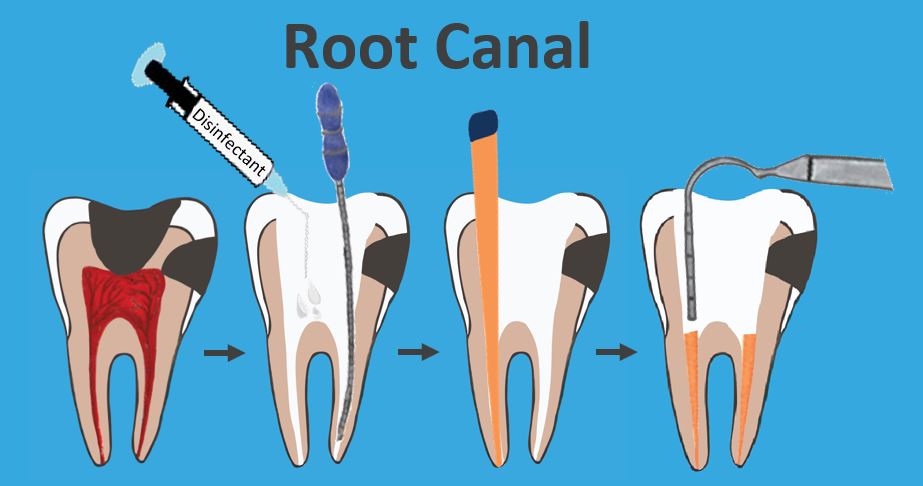
Side Note About Deep Cavities
If a tooth has a deep cavity that extends into the pulp, whether or not it has an abscess, it still needs a root canal.
With very few exceptions that are quite nuanced and beyond the scope of this post to discuss – there is no other way to repair a tooth with decay that extends into the pulp.
It is best to get your root canal done well before an abscess develops. You get to avoid a painful toothache and the prognosis of the root canal is better if there is no infection.
Remember, it’s not the cavity-causing bacteria that cause the abscess. Other pathogenic bacteria are to blame. But the cavity gives those nasty bacteria access right into the pulp. Don’t let that happen if you can help it!
 Treatment Needs After a Root Canal
Treatment Needs After a Root Canal
The root canal takes care of the infected pulp and seals the root. But, that’s it! Your tooth still needs work. Both ends must be sealed and protected to offer a good prognosis
At a minimum, the access hole created to do the root canal must be sealed with a filling. But more often, the tooth needs to be built back up with a large filling called a “build-up.” Sometimes posts are used to secure the filling. After the filling or build-up, the tooth is healthy and cavity-free. Now, we need to address structural integrity.
If it’s a back tooth – any tooth behind your canines – it should be covered and protected with a crown. That is because root canaled teeth are structurally weaker and vulnerable to fracture. Without the crown, the cusps are likely to fracture apart.
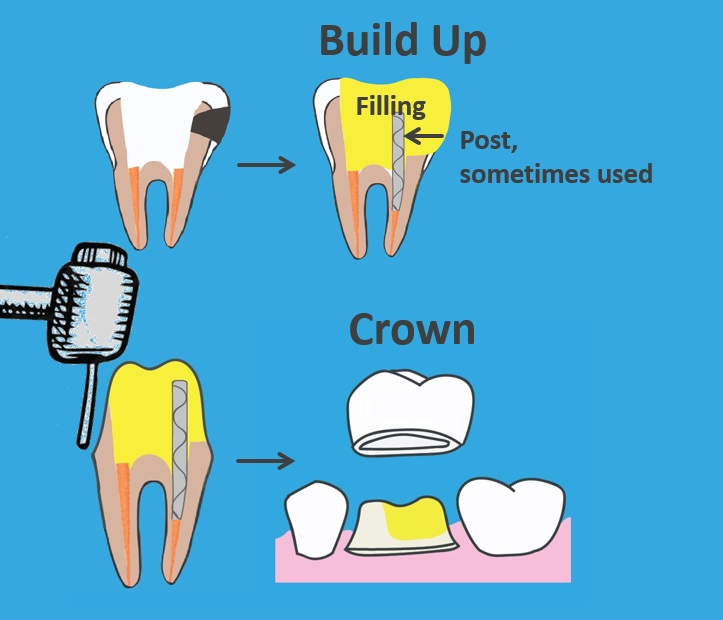
Front teeth are not multi-cusped, so they don’t always need a crown. We only crown front teeth when there is too much damaged tooth structure for a filling to effectively repair.
 This photo shows an example of one of my patients who did not get his crown in time! The fracture was too extensive to save the tooth. We had to extract it.
This photo shows an example of one of my patients who did not get his crown in time! The fracture was too extensive to save the tooth. We had to extract it.
If your tooth already had a crown prior to root canal treatment – good news – oftentimes, you do not need to replace it. We can repair the access hole in your existing crown with a filling.
Specialists are Best!
Root canals can be a tricky procedure. If you need one, your best bet is to see an endodontist – especially if the tooth needing root canal therapy is a molar. Molars have multiple canals and often very complex root anatomy. Endodontists have specialized training in root canals. They devote most of their practice to this one procedure. Their success rate will be higher than a general dentist.
Root Canals Sometimes Fail
Most root canals work the first time. But, sometimes they fail. Either the abscess does not fully resolve or a new abscess develops. The reason is often that there was some portion of the pulp that was not completely removed or effectively sealed off.
Root Canal Re-treatment
Commonly after root canal failure, you can have your root canal re-treated.
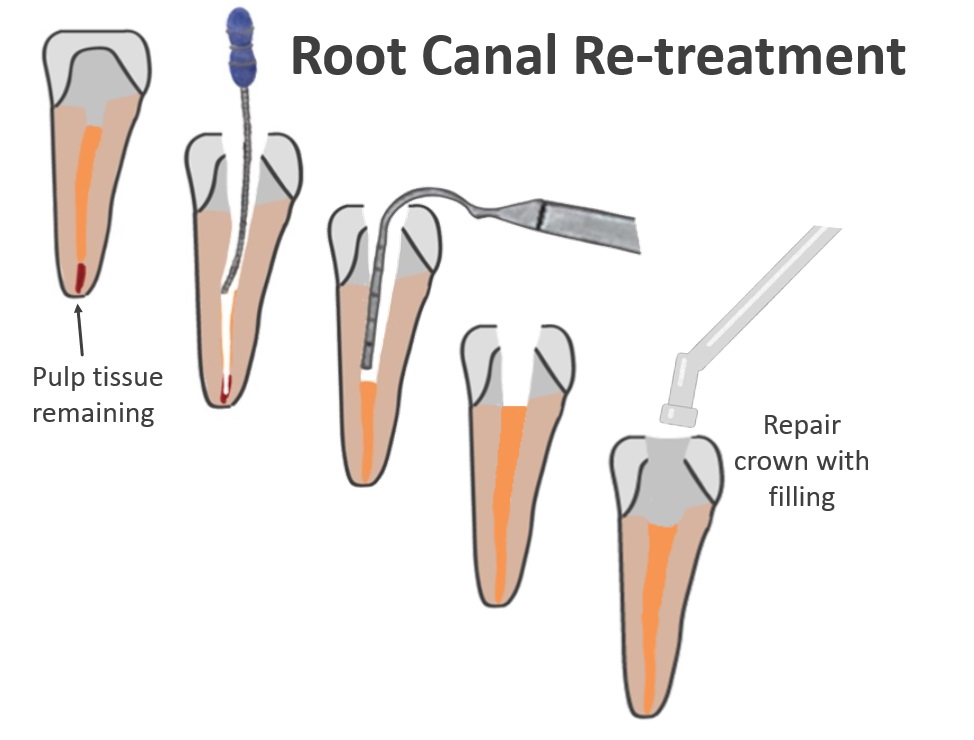
The illustration makes the missed pulp tissue look deceptively simple. It is often not! There can be additional canals and accessory canals that are difficult to see or navigate effectively.
The x-rays below are of a patient of mine who presented with a chronic endodontic abscess. I referred him to an endodontist to have his root canal re-treated, and he’s doing great!
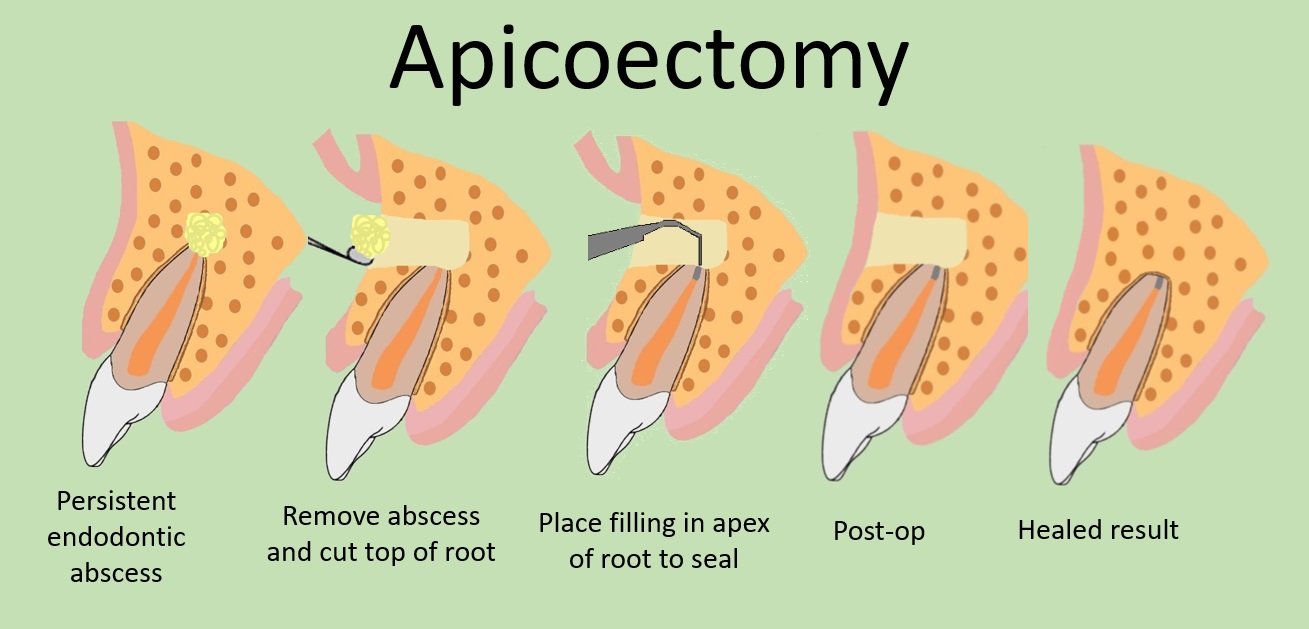
Apicoectomy
Another treatment option to resolve a persistent infection at the tip of the root is called an apicoectomy. Some abscesses are very stubborn. It may be difficult or impossible to resolve with conventional root canal therapy alone. In these cases, dentists or endodontists can sometimes access the tip of the root surgically, remove the abscess, cut part of the root tip off and seal it with a filling.
Other times, after root canal failure, we may determine that it does not have a good prognosis, and we have to extract the tooth. Fortunately, we do have many ways to replace missing teeth. Click here to learn more.
Considerations for Deciding Between Extraction and Root Canal
If you have a restorable abscessed tooth (or a tooth with a cavity that reaches the pulp) you will be faced with the decision to either fix it or extract it.
Factors that influence your decision may include:
- cost – you must factor in the cost root canal plus the cost of the other restorative work needed to fully repair the tooth
- strategic relevance of infected tooth to your chewing function and esthetics
- personal preference – some people have a no-root-canal policy
A Common Scenario
Patients who haven’t been to a dentist in many years are often finally compelled by an abscessed tooth to see me. They often ask me to just focus on the one tooth that is causing the problem. They don’t want me to look at anything else. Presumably, they are trying to save money by doing a limited exam instead of a comprehensive exam.
That is a very bad idea! If I don’t know their overall dental condition, I have no idea whether or not it makes sense to fix the diseased tooth.
What if the patient has ten cavities and needs ten fillings? Does it make sense to spend over $2,000 on a single tooth? Or are they better off spending the same amount of money on the ten other teeth that can be repaired more affordably with fillings? What if the opposing tooth of the abscessed tooth has a hopeless prognosis and needs to be removed? Then the abscessed tooth will end up without a chewing partner, and be less strategic to save.
I think you can see where I’m going here!
I like to offer the best overall dental outcome that a patient’s budget allows. I cannot do that with limited diagnostic information.
My first goal is to get my patients out of pain. I will often numb them if necessary. Nobody is in a good place to make any decisions when they’re in severe pain.
Then, I will do a full exam so that I can help my patients make strategic and informed decisions.
Some dentists don’t insist on the full exam. They’re happy to encourage you to spend a lot of money to repair a single tooth without considering your other treatment needs. Don’t let them.
Be sure you know all of your treatment needs before making a decision. Ask for guidance to focus your dental dollar in the most effective way. You deserve the best overall result that you can reasonably afford.
If you have any questions or comments, post in the comment section below!


What an excellent post on tooth abscess. I had no idea that an abscess could be in the pulp of the tooth or the bone. I just always thought that an abscess was in the gums.
Your article really opened my eyes to the dangers of leaving an abscess untreated for too long. It’s so scary to think that you could possibly die from an abscess.
I have a tooth that flairs up about every three months or so. When it happens, I can’t chew on that side for about two days. I never thought it was an abscess, but maybe it is. I definitely need to make an appointment to see my dentist.
Thank you JarieLyn! If you’re feeling pain to the level that you can’t chew, I would definitely get that checked out. I hope it’s nothing, but better safe than sorry!
Thank you for this informative post. I definitely suffered periodontal abscess. In my early 20’s, I only suffered gingivitis. My gums itched, there was slight pus coming from my gums, and I had bad breath. But I didn’t go to the dentist. When I did, the dentist said if I didn’t address it, it would get worse. I didn’t believe him, and it did get worse.
Fast forward to my 50s. The disease in my gums became so bad, my teeth were loose, I had bad breath, I couldn’t chew food and the bone in my jaw eroded. I had periodontal abscess residing in between the tooth and the periodontal tissues. I had to get ALL of my teeth removed and replaced with all on 4 implants. I’m so happy now. I’m pain free.
Hi Shalista, I’m sorry for all the pain and suffering you have endured. Periodontal disease can really sneak up on people. It’s typically painless until it reaches a very advanced stage. That’s why many patients don’t take it seriously in the early stages. Here is a post where I discuss periodontal disease in more detail: https://informeddentalconsumer.com/your-dentist-said-you-need-a-deep-cleaning-do-you/
I’m glad you’re healthy again. Sounds like you got the top-of-the-line implant supported restoration! I’m so glad that was an option for you. ?