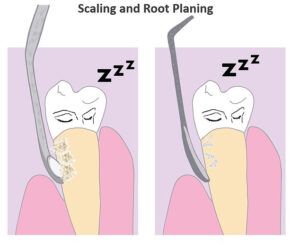
If your dentist or hygienist recently prescribed a deep cleaning, you may be wondering if you really need one. A deep cleaning refers to a procedure called scaling and root planing.
Scaling and root planing is the most conservative and least invasive treatment for periodontal disease. It involves scaling deposits of plaque and tartar off your tooth surfaces and smoothing the roots to create a surface less conducive to plaque accumulation. Often times you are numbed with a local anesthetic for the procedure.

To determine whether this treatment is appropriate for you, it helps to understand more about periodontal disease.
What is Periodontal Disease?
First, let’s break down the word periodontal. In a medical context, “peri” means all around and “dontal” means teeth. So periodontal refers to the tissues that are all around your teeth. More specifically, the gums, bone, and ligaments that are holding your teeth in place – everything but the teeth themselves. Periodontal disease – also called periodontitis or gum disease – is an inflammatory condition that damages those tissues.
Plaque is the Enemy
Plaque is a sticky film comprised of bacteria and bacterial byproducts. It is to blame for most dental problems. If plaque is not removed in time, it can harden and turn into calculus. Calculus is that chunky stuff you call tartar.
There are hundreds of different species of bacteria in our dental plaque. Only some of these species trigger the destructive immune response of periodontal disease. Others cause cavities and others don’t cause any harm. Your susceptibility to periodontal disease, calculus build-up, and cavities is heavily influenced by which bacterial species comprise your plaque as well as your immune response and general health.
Yep, it’s a little unfair. Our baseline susceptibility to dental disease is influenced by many factors beyond our control. That’s the bad news. The good news is that you have some control too. The factors under your control include your diet, your health habits, your homecare routine, and the frequency of your professional dental cleanings.

Teeth are Required
Even though teeth are not part of our periodontal tissues, teeth must still be present to develop periodontal disease. That is because damaging bacteria make their home in-between the teeth and the surrounding tissues. If teeth are not present, there is no place for the plaque and calculus to settle.
If plaque and calculus are not cleaned out regularly, they can trigger inflammation, and eventually the destruction of periodontal tissues. The damage occurs in stages.
Gingivitis
Gingivitis is a precursor to periodontal disease. With gingivitis, the gums become inflamed. They get puffy, swollen, and bleed easily. But there is no bone loss.
Inflammation is the body’s natural response to irritants. But, in the case of periodontal health, inflammation can work against you. That’s because puffy and swollen gums create more hiding places for the bad bacteria.
The plaque bacteria are what triggered the inflammatory response in the first place. And, now the puffy gums are harboring more plaque. It’s a terrible feedback loop. Fortunately, with the right care, plaque-mediated gingivitis is usually reversible. You just need to treat it in time. It is usually solved with regular professional cleanings and better home care.
Official Periodontal Disease
If you don’t reverse gingivitis, the stage is set for periodontal disease. Periodontal disease is defined by the loss of supporting bone. It can be very localized – only affecting a few teeth – or it can be generalized and affect most or all of your teeth.
Inflammatory Immune Response
Our immune system has good intentions. It sees invaders and wants to attack. Unfortunately, it can go awry. In the case of periodontal disease – instead of effectively attacking the bacteria – it attacks the surrounding tissues. It destroys the gum-tooth attachment apparatus and the supporting bone.
As a result, deeper crevices form between the teeth and the periodontal tissues. More and more plaque and calculus accumulate. The feedback loop continues and the effect snowballs.
Diabetics and Smokers
If you have uncontrolled diabetes or you are a smoker, you are more susceptible to periodontal disease. For these populations relatively small amounts of plaque and calculus trigger this dysfunctional inflammatory immune response. To make matters worse, they often have a compromised blood supply to their periodontal tissues. It is more difficult for damaged tissue to heal.
Prevalence and Progression
Periodontal disease is much more common than many people realize. Half of all adults over 30 have some level of periodontal disease. As you get older your risk increases. Click here to learn more.

Periodontal disease progresses through increasing levels of severity. For most people, it progresses slowly over the course of many years – sometimes decades. In the early stages, when it is much easier to treat, it typically does not cause pain or other noticeable symptoms. Therefore, those who do not see a dentist regularly are not compelled by pain to seek treatment.
In advanced stages, periodontal disease becomes symptomatic. Teeth become mobile and chewing is painful. Some people – even those who are not prone to cavities – start to develop many new cavities. That is because bone loss exposed root surfaces to cavity-causing bacteria inside the mouth. Root surfaces are seven times softer than enamel and much more vulnerable to cavities.
The x-ray below shows a patient of mine who finally sought dental care when he developed toothaches from large cavities that resulted from root exposure.


Sometimes the bacteria harbored between the teeth and the gums actually find their way into the pulp of the tooth and cause a terrible toothache. In such a case, if the tooth can be saved, it would require a root canal in addition to the appropriate periodontal therapy.
In the last stage of gum disease, teeth are floating in puss. Sometimes they fall out on their own.
When these sorts of consequences happen, folks are compelled to seek treatment. Of course, by this point, it’s very difficult or impossible to treat. It is much better to treat periodontal disease as early as possible.
Believe it or not, these are not the only consequences of periodontal disease, nor are they the most serious. The biggest concern of gum disease is the effect it may have on your general health.
Systemic Health Impact
There are many health problems and diseases that have been linked to periodontal disease. Here are some examples.
- Heart Attacks
- Strokes
- Diabetes Complications
- Ulcers
- Pre-term Low Birthweight Babies
- Alzheimer’s Disease
- Some forms of Cancer
The research in this area is ever-evolving. But, it certainly stands to reason that periodontal disease can have negative consequences for your general health.
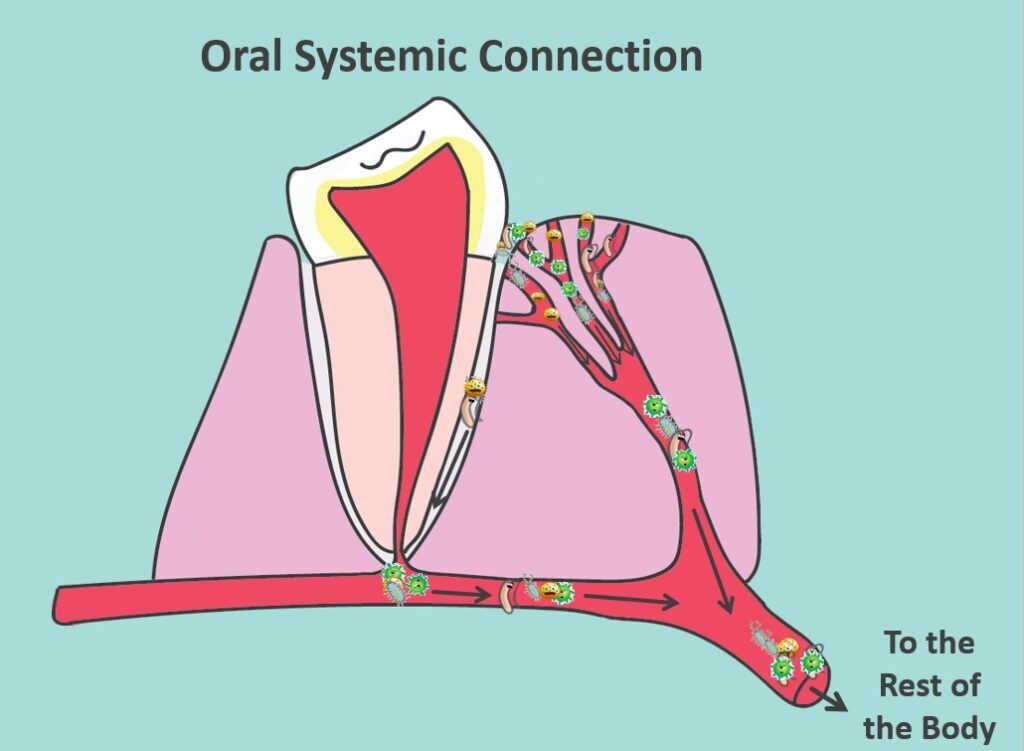
The toxic bacteria in your dental plaque and inflammatory byproducts of your immune response can get into your bloodstream. They can cause blood clots, or otherwise, wreak havoc on your body.
Transmissibility
It turns out that the more pathogenic bacterial species – the ones that most readily trigger the destructive immune response of gum disease – can be transmitted from person to person, even as adults. Once gum disease develops, the amount of bacteria in your mouth is exponentially greater. You will have more potential to transmit them to your loved ones. So, treating your gum disease may not only benefit you, it may protect your loved ones as well.
 Statement from the American Academy of Periodontology
Statement from the American Academy of Periodontology
“… the bacteria that cause the inflammatory reaction [of gum disease] can be spread through saliva. This means that if one of your family members has periodontal disease, it’s a good idea to avoid contact with their saliva by not sharing eating utensils or oral health equipment.”
I hope it’s now clear how important it is to diagnose and treat periodontal disease as early as possible!
How Do We Diagnose Periodontal Disease?
Hard Tissue Assessment
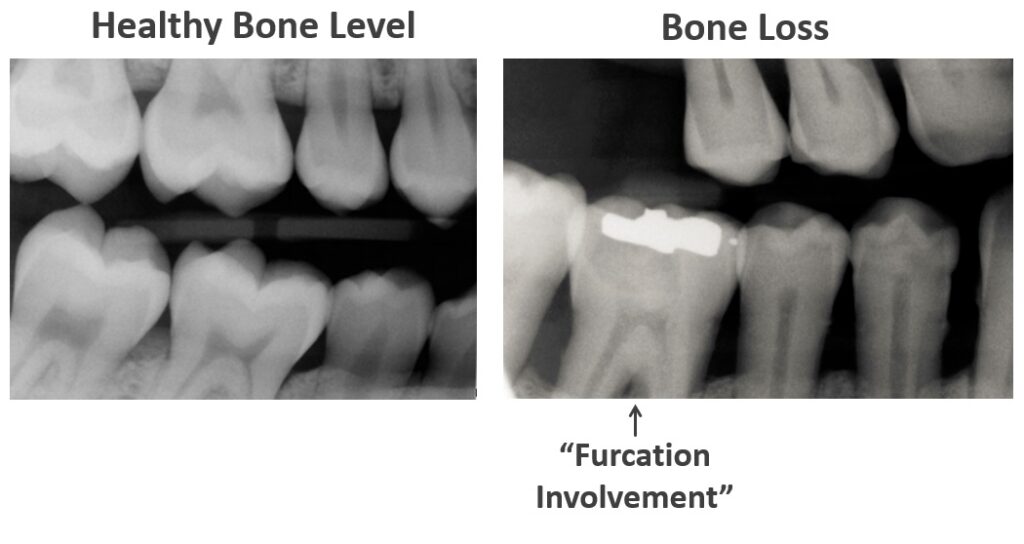
One of the tools we use to assess your periodontal health is dental x-rays. They show us your bone level. The x-ray on the left shows a healthy bone level while the x-ray on the right shows bone loss as a result of gum disease.
Sometimes x-rays show us that a tooth root’s dividing point is now exposed to the oral cavity when it used to be buried in bone. That’s called a furcation involvement. A furcation involvement makes the tooth harder to maintain in the long term because plaque can settle in that tough-to-reach location between the roots.
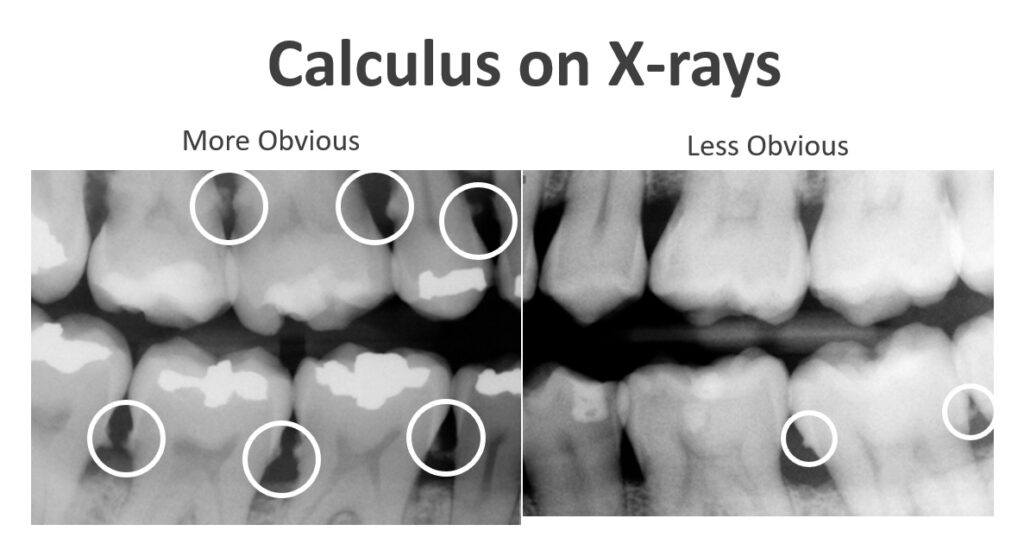 X-rays may also show us spikes on your teeth. These spikes are actually calculus build-up. Remember, calculus is just plaque that has been sitting around a while and hardened. If it’s visible on a dental x-ray, even just a little bit, it’s a sign that you have heavy calculus build-up. It takes a lot of build-up before it shows up on an x-ray.
X-rays may also show us spikes on your teeth. These spikes are actually calculus build-up. Remember, calculus is just plaque that has been sitting around a while and hardened. If it’s visible on a dental x-ray, even just a little bit, it’s a sign that you have heavy calculus build-up. It takes a lot of build-up before it shows up on an x-ray.
Unfortunately, calculus serves as a sticky matrix that attracts a lot more soft plaque. And, that plaque can start to harden into even more calculus.
Soft Tissue Assessment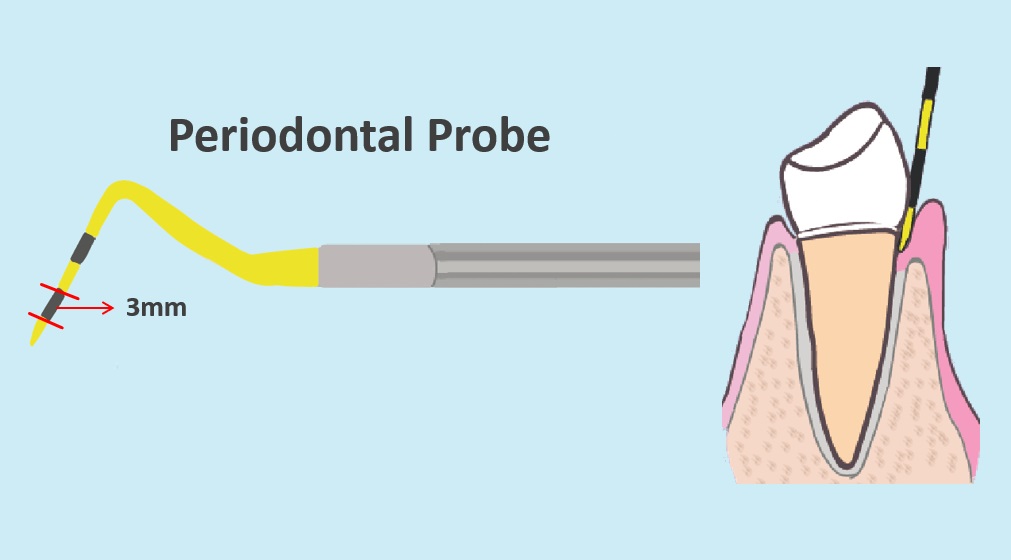
We can’t rely on x-rays alone to assess your periodontal health. X-rays only show only hard tissue. Sometimes people have experienced bone loss from gum disease, but the disease is now controlled and the tissues are now healthy.
In order to assess the actual soft tissue destruction, we use an important but simple diagnostic tool called a periodontal probe.
We use it to measure the extent to which the gums have detached from the tooth. If there is no, or minimal soft tissue destruction, it won’t sink down very far. However, if gum disease has destroyed some connective tissue, it will sink further down. It’s like golf. Lower numbers are better.
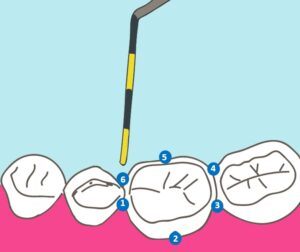 To get the full picture, we measure six places around each tooth. These sites are referred to as periodontal pockets.
To get the full picture, we measure six places around each tooth. These sites are referred to as periodontal pockets.
Generally speaking, pockets between one and three millimeters are healthy. A four-millimeter pocket is either early disease or reversible tissue swelling. Five to six-millimeter sites usually need attention and treatment. Above six millimeters it gets tougher to treat. But these are guidelines. It can be a bit more nuanced.
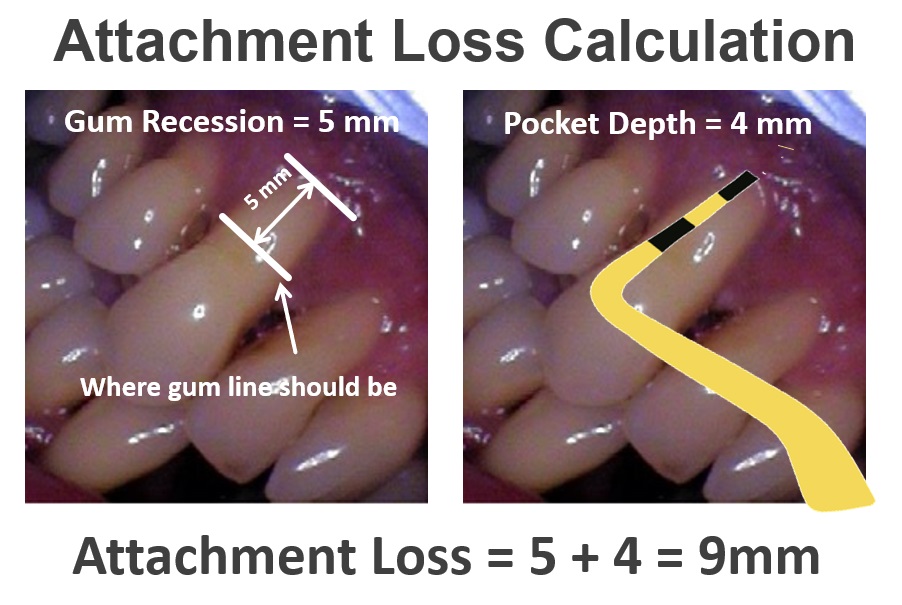
Sometimes we need to add the tissue recession, as represented on the left, to the pocket depth. And together they equal what we call attachment loss.
There are many factors besides just probe depths alone that inform our treatment planning. But probing is essential. Sometimes, the probe depths offer the only clue that gum disease has developed.
Believe it or not, if your gum tissue is healthy, we can insert the periodontal probe into the pocket, and it won’t hurt or bleed. Wherever the probe elicits bleeding is identified as an inflamed area. If you have a deep pocket that consistently does not hurt or bleed on probing, that suggests that the tissues are healthy in that area despite the deep pocket. Bleeding on probing is an important piece of diagnostic information.
One caveat for smokers – for smokers, bleeding may be less evident despite advancing disease. Again, they often have a reduced blood supply to peripheral tissues and their periodontal disease can be masked by a lack of bleeding. 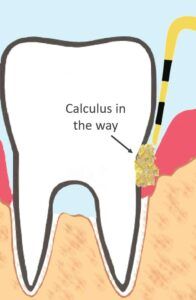
If you have a lot of calculus build-up, we may not be able to get accurate probe measurements right away. We may need to remove the interfering calculus first. The severity of disease, and the full scope of treatment required, will not be determined until we know your pocket depths.
How Do We Treat Gum Disease
 Teeth Extraction
Teeth Extraction
One surefire way to eradicate gum disease is to remove teeth affected by gum disease. Tooth removal is the only known cure for gum disease. For obvious reasons, it’s not our first choice. But sometimes it’s unavoidable or it just makes the most sense. Once the teeth are gone, the toxic bacteria have no place to live. Again, their home is between the teeth and gums. When the teeth are gone, they move out.
Unfortunately, there are many folks who have had all of their teeth in one or both jaws claimed by gum disease. They usually have to replace them with dentures. Fortunately, there are better full tooth replacement options than conventional dentures. But these are more expensive and inaccessible to many people. 
Often, instead of removing all of your teeth, we just remove the teeth in the worst condition and replace them. To learn more about the different ways we replace missing teeth click here.
Sometimes, it makes sense to remove teeth that are what we call “non-strategic.”
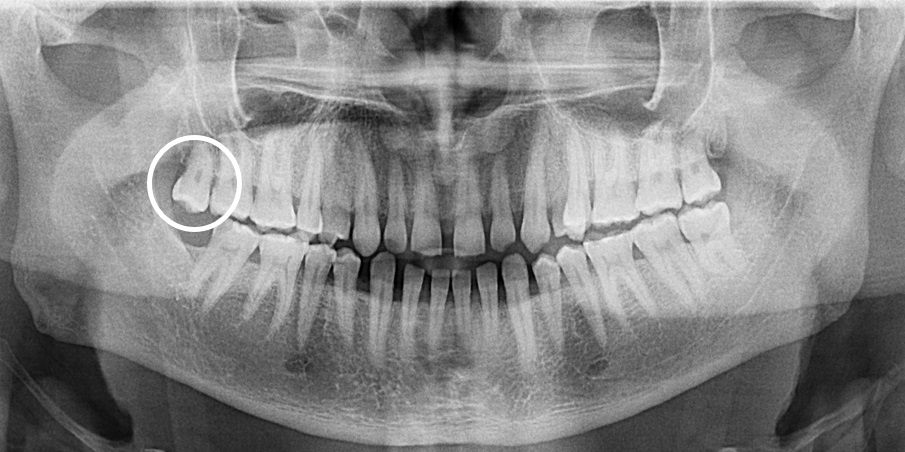
The x-ray above shows an example. This circled tooth has no function or value. The only thing this tooth is good for is harboring more bacteria. So let’s get rid of it. This is low-hanging fruit in the management of gum disease.
Terminal Teeth
A tooth with gum disease can be terminal in a sense. We might know that it’s past the point of no return. But it might hang on for months or years before it’s actually lost. So, it’s tempting not to do anything. That tooth is still there chewing without any pain, so it doesn’t seem like an issue. Unfortunately, while it’s still there, it’s sustaining your chronic inflammatory disease and potentially damaging your systemic health. It’s also negatively impacting the neighboring teeth. The excessive bacteria could easily start to infect the neighboring pockets. I am in favor of proactive tooth removal in these cases – both to protect your general health and your other teeth. It’s a bad idea to keep a tooth held in by hopelessly diseased tissue just because it doesn’t hurt.
Periodontal Therapy
Aside from tooth removal, there is no cure for periodontal disease. However, as long you haven’t passed the point of no return, we can manage it. We can’t get back all that was lost. You will have permanent anatomical changes favoring greater plaque and calculus accumulation. But, in many cases, we can create an oral environment where you are just as healthy as someone without gum disease. You’re just going to need treatment beyond a preventative cleaning, and you will need more frequent ongoing attention.
Specialty Procedures for Advanced Periodontal Disease
Surgical Therapies
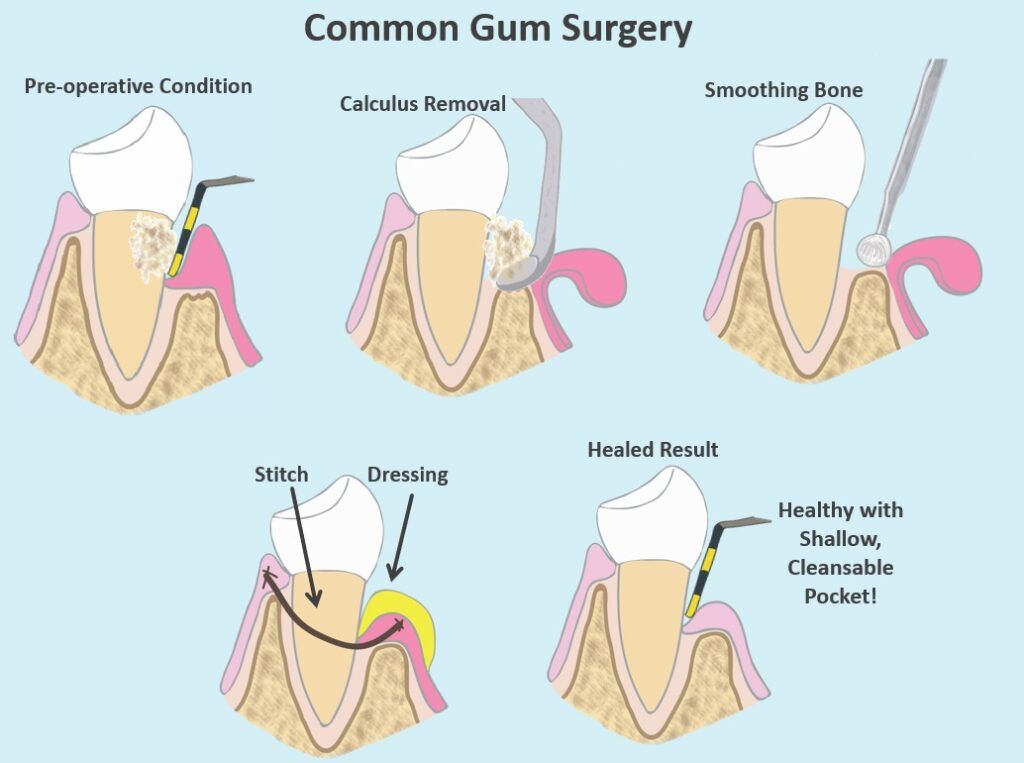
For more advanced stages of periodontal disease, surgical therapies are available. They are typically performed by a dental specialist called a periodontist. A common surgery is shown in the image above. It involves exposing your teeth and bone with a surgical flap. The flap allows the surgeon much better access to remove the calculus build-up between the teeth and the gums. The gums are sewn back up in such a way that your pockets are reduced. When it’s finished, your teeth will look longer, because the gums are going to be secured down closer to the bone. But you won’t have such deep pockets under the gums for the plaque and calculus to hide. It will be much easier for you and your dentist or hygienist to keep these areas clean.
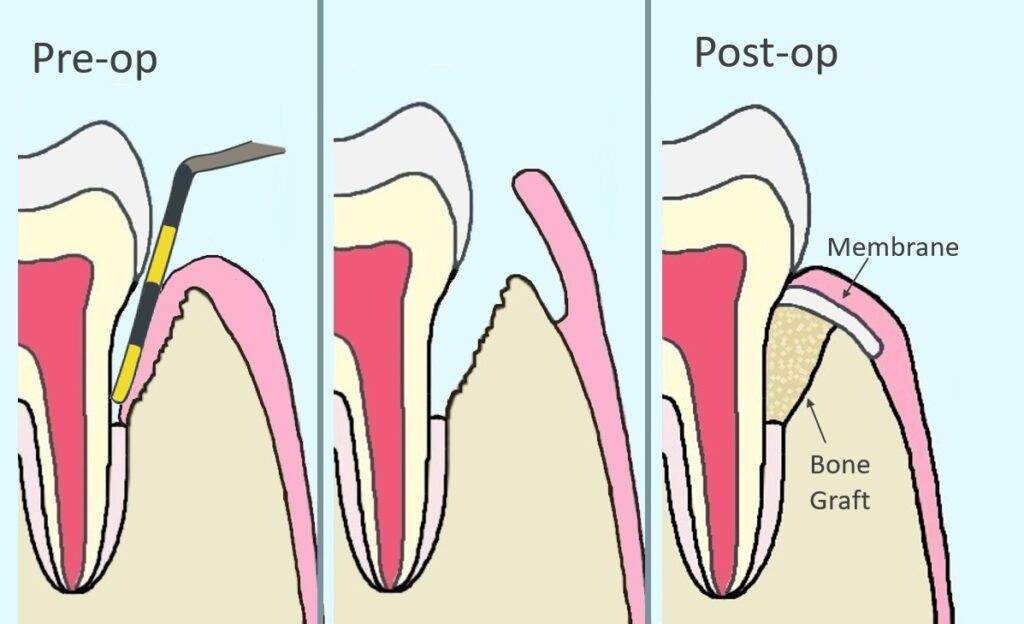
Another surgical option is represented in the above image. It is a grafting procedure called guided tissue regeneration. It requires walled bony defects that are amenable to grafting. If your bone loss is horizontal, it won’t work. The intention is to rebuild your periodontal anatomy and reduce your pocket depth.
Nd YAG Laser
A more recent development in periodontal therapy is the use of a special laser called the Nd YAG laser. Lasers can emit targeted and concentrated energy and kill the infection without damaging healthy tissue. It is less painful than traditional surgery and has shown great results. There are other lasers used in dentistry, but the Nd YAG has shown great promise for specifically for periodontal disease.
The main downside of these specialty procedures is the cost. They can be out of reach for many patients.
Mild to Moderate Periodontal Disease Therapies
Scaling and Root Planing
Now we’re back full circle! You wanted to know if you needed the scaling and root planing described at the beginning of this post. Scaling and root planing is most appropriate for those with mild to moderate periodontal disease. If that is all you need, feel lucky! Again, in this procedure, your hygienist or dentist will use conventional dental scaling to access the plaque and calculus in your periodontal pockets.
Do You Need it?
As a rule of thumb, I am much more concerned about patients who decline scaling and root planing when they really need it than vice versa. Conservative periodontal treatment is not an area to nickel-and-dime your care. That said, it is perfectly reasonable to ask your dentist to show you the evidence that the scaling and root planing procedure is indicated. I hope you better understand what we’re looking for.
- 4mm+ deep periodontal pockets
- Bleeding on probing
- Radiographically visible bone loss
- Calculus build-up
After you complete scaling and root planing, you are not finished. You are never finished! Practice good home care and follow up with professional maintenance cleanings. Hygiene recalls are forever (and ever and ever!)
Periodontal Maintenance
We refer to your recall cleanings as Periodontal Maintenance. Periodontal Maintenance is much easier, faster, and cheaper than scaling and root planing. You are typically not numbed for the procedure. It is similar to a preventative cleaning, except that we will scale any new plaque and calculus that have found their way into your periodontal pockets. We also more closely monitor the depth and bleeding of your pockets at each visit. If your pockets get deeper or do not respond to conservative treatment, additional therapeutic intervention may be needed.
If you are not committed to regular periodontal maintenance after your scaling and root planing, then you might as well skip the scaling and root planing. While good home care with regular brushing and flossing is critical, it’s not enough to remove the plaque and calculus embedded deep inside the periodontal pockets. They’re like cookie crumbs in couch cushions. They’re impossible to clean out without professional intervention. More plaque and calculus will find their way in there every day. You wouldn’t clean your kitchen once and think you’re done for life. The kitchen gets dirty again, and so do your teeth. The standard of care after scaling and root planing is to have periodontal maintenance cleanings every three months.
Adjunctive Therapies
If you need more than just scaling and root planing, but you are not a candidate for a specialty procedure, or you cannot afford the specialty procedures, you can try an adjunctive therapy.
Antibiotic Chip
One option is to have an antibiotic chip placed inside your deep periodontal pockets. A popular one is called Arestin. It contains minocycline which is in the tetracycline family. Minocycline is targeted toward the bacteria that cause periodontal disease. It is nicer to embed the antibiotic in your periodontal pocket than to take a pill. It allows us to use a very tiny 1 mg dose – far less than the pill form – and it will only affect the targeted area. With such a tiny dose, the systemic impact will be negligible. You will often need to repeat the chip application periodically at your hygiene visits to sustain the results.
Diode Laser
Another option is to use a diode laser beam to kill the bacteria in your pocket. This procedure is called Laser Assisted Bacterial Reduction and is typically done during your periodontal maintenance visits. It only takes 5 to 10 minutes and requires no anesthetic. Studies on this procedure show mixed results. However, it certainly won’t hurt, and it might help.
Perio Protect Tray
These are custom-made hygiene trays. They are designed with your pocket depths in mind. The trays are used to deliver a special, minty, bacteriocidal gel into the depth of your periodontal pockets. You typically wear these trays for 15 minutes at least twice per day for best results. It requires some compliance and commitment. But, your mouth feels great after using them and it might be an affordable way to avoid the more costly procedures. A nice side effect is that the gel also bleaches your teeth. Click here to learn more.
Response to Therapy
I wish it was one-size-fits-all. But the truth is that everyone responds differently to periodontal therapy. Many will have an excellent outcome and some won’t. Again, your maintenance cleanings are critically important. Not only do we need to clean new plaque and calculus, but we will also continually monitor your condition so we can intervene with another approach when necessary.
Prevention
The tragedy for most sufferers of periodontal disease is that it is usually completely preventable. The reason that most people develop periodontal disease is that they did not access (or have access to) regular professional dental cleanings. We know – life happens and dental care can end up on the back burner.
But you don’t save money by avoiding the dentist. Uninsured out-of-pocket cost for preventive care is cheaper than managing insurance co-pays and overruns for bigger procedures. Not to mention, the clinical outcomes of prevention are so much better.
Coding and Billing
Since we are cost-focused here at Informed Dental Consumer, here is some information to help you understand the appropriate fees for scaling and root planing.
When coding for periodontal therapy, we divide the mouth into four quadrants – upper right, lower right, upper left, and lower left. You pay a fee for each quadrant.
There are two codes for scaling and root planing.
D4341 means that four or more teeth in the given quadrant require scaling and root planing
D4342 means that three or fewer teeth in the given quadrant require scaling and root planing
When you view your treatment plan, you will see the quadrant and the code identified. For example:
- UR D4341
- LR D4342
- UL D4342
- LL D4341
Of course, D4342 is a little less expensive than D4341. If your periodontal disease is mild, you can ask your provider if the less expensive D4342 would be appropriate.
After you complete scaling and root planing, you will follow up with Periodontal Maintenance regularly. The procedure code is D4910. Most insurance plans will cover periodontal maintenance every three months or four times per year. They usually contribute 80% after your deductible is met.
Research these codes at the Fair Health Consumer website to determine what fees are appropriate for you.
Finally – the Answer to Your Question
My statistically-informed guess based on twenty years of experience as a dentist is that you probably do need scaling and root planing if your dentist or hygienist recommended it. Best of luck with your dental care, whatever you decide!
Please feel free to comment below if you have any questions, or would like to share your experience.



Thanks for all this information on dental care. I didn’t know that smokers and person suffering from diabetes more susceptible to periodontal disease. I am shocked to find out that there are many health problems and diseases that have been linked to periodontal disease. You have me doing some introspection. I have to take better care of m teeth after reading this. To know that bacteria can get into your blood stream is scary, and cause so much harm, even death.
Hi Shevonne! Yes, oral health can sometimes be overlooked as a contributor to your general health. I’m glad to hear that you will be working on your dental care. Healthy mouth = healthy body! Thank you for your thoughts.
Wow, that is an excellent write-up on cleaning your teeth. I have my teeth professionally cleaned and polished every 6 months give or take. I have had scaling done and was happy with the results. My issue is with the billing these dentist try to pull off. When I get my bill I always look at what they charge the insurance company. They always try to get away with charges they shouldn’t. Hence why I have been looking for a honest dentist.
Hello Chris! I’m glad you’re going for professional cleanings regularly. If you had a deep cleaning done at some point in the past, your hygienist should be re-evaluating your pocket depths at your recall visits. Re: billing, I’m not sure what they are doing, but, if you are in the United States, the typical protocol is to use the periodontal maintenance code, D4910. There are some of the adjunctive therapies I mentioned. Maybe they’re doing that too? But, whatever they’re doing, they should get your approval and buy-in first. But, most importantly, just be sure to keep going!
Hi Beth,
What a helpful site! Great content! I personally went through Periodontal Disease over 25 years ago. The procedure and having my mouth opened for sooooo long during surgery scared me straight to take better care of my gums. I just naturally have one of those mouths that is a plaque factory. So, I learned the wonderful practice of flossing after brushing morning and night before bed. At night after brushing and flossing, I also use a GUM Stimulator Permanent Handle with Rubber Tip. Doing this for years now is keeping me away from cavities. I used to be one of those guys when he went in for a check up would have 1 to 3 cavities. It’s a wonder I still have my teeth. I had all my fillings redone and now my teeth are in pretty good shape according to my dentist. My father had the same problem and he ended up needing false teeth. And I was not interested in that one bit : ).
Keep up the good work Dr. Beth!
All the best,
Paul
Hi Paul! Thank you! I like that term – Plaque factory. LOL! Yes, some people are like that, including me. I build up very easily too. It’s really not fair! Some people hardly develop any plaque. It is not necessarily because they’re doing a better job with their home care. There are just differences in oral chemistry from person to person.
I’m glad you haven’t had any cavities lately, and that you’re in much better shape! Keep it up!!!