It’s frustrating to feel pain on a tooth that wasn’t hurting before you had a filling or crown placed. But, it doesn’t necessarily mean that your dentist did something wrong. I hope to make sense of why this can happen and what your dentist needs from you to make a diagnosis.
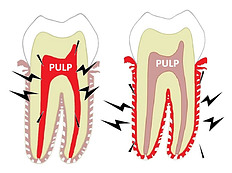
The pain you’re experiencing comes from either the pulp of the tooth – the part where the sensory nerves are located – or it comes from inflamed tissues around the tooth. Or both.
Signs vs Symptoms
Sometimes we can rely on signs to make a diagnosis and treatment decisions. Signs refer to phenomena that an outsider can detect. But, often times we need to take into account your symptoms. Only you can experience your symptoms. We’ll often be relying on your description of those symptoms to help determine our diagnosis.
Three Causes of Tooth Pain After Fillings or Crowns
- High bite
- Reversible pulpitis
- Irreversible pulpitis
High Bite 
A common mistake we dentists make is leaving your tooth too high. We might pack your filling too high, or make your crown too tall. We try to achieve the optimal bite, but sometimes we don’t adjust quite enough.
When this happens, of course, your tooth is taking the brunt of your biting force. This situation can be particularly problematic for clenchers and grinders. The trauma of the high bite can aggravate the pulp and/or the tissues surrounding your tooth. Fortunately, this problem has an easy fix – a bite adjustment.
But, not everyone is so lucky. There are other reasons that a tooth develops pain after dental work. And, these reasons are typically about the pulp.
Pulpitis – Reversible vs Irreversible
The trauma of the dental work can sometimes cause the pulp to become inflamed. An inflamed pulp is called pulpitis. Deep fillings and crown preparations have a greater chance of triggering pulpitis than shallow fillings.
An inflamed pulp sends pain signals – either for no reason at all or at the slightest provocation. After pulpitis develops, the pulp can either recover or die.
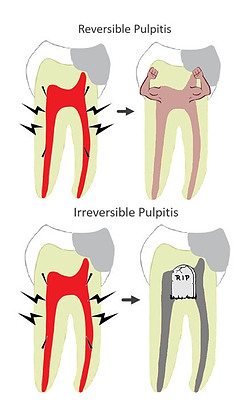
If your pulp is inflamed but we expect that it will recover – you have reversible pulpitis. The majority of postoperative pulpitis is reversible.
If we expect that your inflamed pulp will not recover, you have irreversible pulpitis.
It’s important to distinguish the pain caused by simple reversible pulpitis from the pain caused by an infected pulp, or irreversible pulpitis.
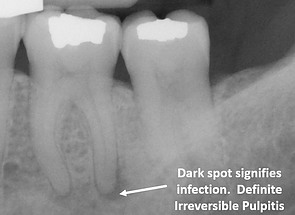
A certain sign of irreversible pulpitis would be to see a dark spot at the tip of your root on an x-ray like the one pictured. If we see that kind of lesion on your x-ray, we won’t need to ask you any questions. We would know right away that your pulp is infected.
But more often we don’t get such diagnostic certainty. We will be relying on your description of your symptoms to get our answer.
Reversible Pulpitis Symptoms
The pain caused by reversible pulpitis is usually triggered by a stimulus like a temperature change, chewing, or sweets. The pain quickly subsides when the stimulus is gone. It’s not entirely cut and dry. A tooth with reversible pulpitis can have some unprovoked pain, but that usually resolves within a few days after the work was done.
Generally speaking, the tooth is not keeping you awake and making you absolutely miserable. It just hurts when you’re eating, brushing your teeth, or maybe breathing in cold air on a winter day. As soon as you stop, the pain resolves.
So, your textbook reversible pulpitis pain is triggered by a stimulus and stops quickly after the stimulus is gone. If your pain is behaving that way, then we have good reason to expect that your pulp will recover. Your tooth should become less and less sensitive over the next few weeks to months.
Irreversible Pulpitis Symptoms
Textbook irreversible pulpitis is characterized by high, unprovoked pain or lingering pain after a stimulus.
Unprovoked Pain
Unprovoked pain is the kind of pain that you feel when you’re sitting around doing nothing. You’re not necessarily chewing or exposing your tooth to a cold drink. The tooth just plain hurts! And the pain is at a high enough level to prevent you from sleeping. By the time you’re jarred awake with pain and throbbing, the infection has usually gone beyond the pulp and into the surrounding tissues. That is why it hurts so badly.
Lingering Pain After Stimulus
Irreversible pulpitis doesn’t always cause unprovoked pain. Sometimes it is only triggered by a stimulus like hot or cold temperatures, chewing, or sweets. But unlike reversible pulpitis, the pain does not disappear quickly after the stimulus is removed. It hangs around for a while – maybe 30 seconds or more. Sometimes we test the pulp by applying a cold stimulus to the tooth and see how long it takes for your pain to disappear. (Sorry!)
If your symptoms are severe enough, they alone can point us to a diagnosis of irreversible pulpitis. We may not see any objective signs of a pulp infection on your x-ray or in your mouth. Just the description of the pain you’re experiencing may be enough to convince us that you have irreversible pulpitis.
Why Would My Filling or Crown Cause Irreversible Pulpitis?
Actually, it doesn’t! Sometimes, dental work can ramp up a pre-existing, low-grade infection. Your filling or crown was done on a tooth that was already afflicted with irreversible pulpitis. We just didn’t know it.
There are plenty of dead and dying pulps in the world. We don’t necessarily know the status of a pulp unless we either intentionally test the sensory abilities of the tooth, or if the pulp develops an infection. It is the latter reason – an infection – that usually gives rise to the diagnosis of irreversible pulpitis. By the time we diagnose you with irreversible pulpitis, your dead or dying pulp is filled with toxic bacteria.
The dental work didn’t cause the infection. It just put gasoline on the fire. Click here to learn more.
Irreversible Pulpitis Treatment
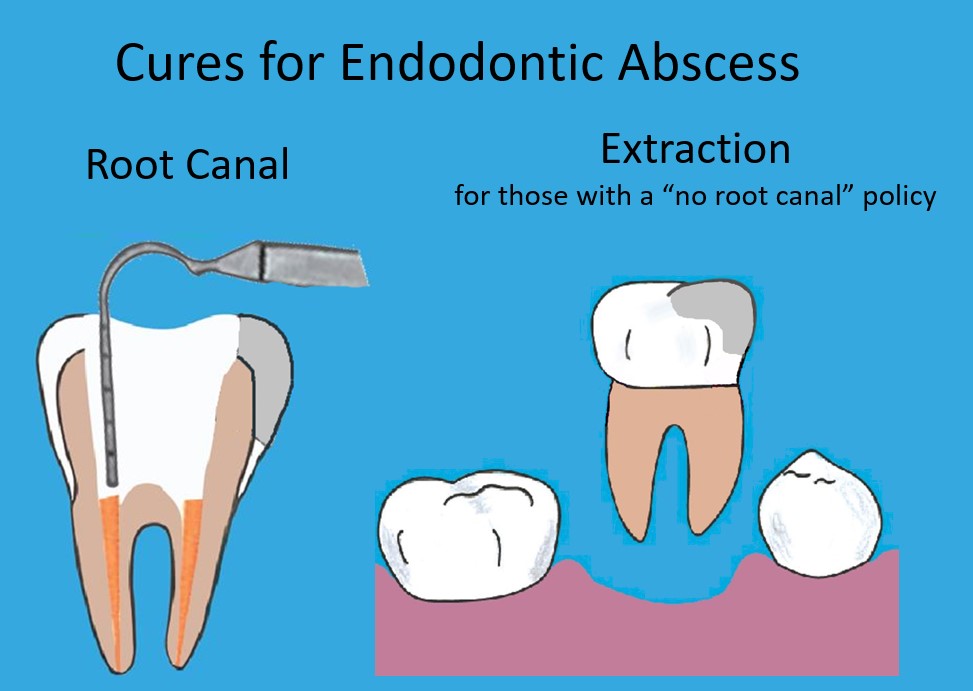
If you do have irreversible pulpitis, your infected pulp tissue needs to be cleaned out of the inside of your tooth, and a filling must be placed inside your root where your pulp tissue used to reside. In other words, you need a root canal.
If you don’t want to have a root canal, or your dentist does not think root canal treatment offers a good prognosis, the only other treatment option for irreversible pulpitis is to have your tooth removed.
Antibiotics – Not the Answer
If you have irreversible pulpitis, antibiotics will not solve your problem. Antibiotics are never, ever, ever a cure for an infected pulp. It’s important to definitively take care of the tooth infection as soon as possible.
Dentists often prescribe antibiotics as a short-term band-aid. It is thought that antibiotics reduce the infection so that your pain is more manageable for a week or two while you’re waiting for your appointment. But that assumption has been called into question. Click here to learn more. Antibiotics may be needed prior to treatment if you have significant swelling – the kind a stranger would notice. We like to reduce that kind of swelling before we do root canals or extractions.
Real World Diagnostic Uncertainty
As it turns out, determining whether or not you have reversible pulpitis or irreversible pulpitis is not always so clear-cut in the real world.
If the filling or crown was pretty recent and your symptoms are borderline, we may just need to wait and see if the tooth calms down, or gets worse. Or, we will refer you to a specialist called an endodontist. Endodontists typically have cone beam imaging capabilities. Sometimes these 3d images will pick up a dental infection when x-rays can’t.
The good news is that of the three causes of post-operative tooth pain,
- a high bite,
- simple reversible pulpitis, and
- irreversible pulpitis
irreversible pulpitis is the least common.
Hopefully, you’re now in a better position to help your dentist figure out what might be going for you. I sure hope it gets better soon! If you have any questions or want to share your experience with tooth pain after dental work, please share in the comment section below.


As a dental assistant, I am so grateful for an article like this. I actually learned one or two things as well,which will help me to better serve my patients.
Most importantly, however, when a patient is equipped with knowledge like this, their treatment will typically be much more effective because they are able to communicate the information we need to know to help provide the correct treatment.
I think everyone should check out this information! Not just when they start to get a toothache, but beforehand, when they can maintain awareness of something changing in their mouth.
Keep up the great work!
Thank you so much, Ashley! I hope you can use these posts to educate your patients. I’m sure your office does many fillings and crowns, so you’re sure to have many patients with pulpitis afterward.